ABSTRACT
Classical Ehlers-Danlos syndrome (cEDS) is one of the 13 subtypes of Ehlers-Danlos syndrome, which has the major clinical criteria of hyperextensibility skin, atrophic scars, and generalised joint hypermobility. The occurrence of aortic dissection has been described in some subtypes of Ehlers-Danlos, but it has a rare association with the cEDS subtype. This case report discusses a 39-year-old female with a past medical history of transposition of great arteries with a Senning repair at the age of 18 months and controlled hypertension with medication, who presents a spontaneous distal aortic dissection. The diagnosis of cEDS was made using the major criteria, and a novel frameshift mutation in COL5A1 was discovered. The reported case emphasises that in patients with cEDS, vascular fragility may be a complication.
LEARNING POINTS
- Classical Ehlers-Danlos is a rare autosomal dominant inherited connective disorder.
- Arterial dissections are rarely found in cEDS patients.
- Association of cEDS and vascular fragility can result from new type V collagen mutation.
KEYWORDS
Classical Ehlers-Danlos syndrome, aortic dissection, COL5A1 mutation
INTRODUCTION
Ehlers-Danlos syndrome (EDS) comprises a group of inherited connective tissue disorders (CTDs) characterised by a defect in the synthesis or the structure of collagen. To date, there are 13 EDS subtypes that exhibit genetic, phenotypic, inheritance patterns and molecular variations[1].
Classical Ehlers-Danlos (cEDS) is a rare autosomal dominant inherited connective disorder characterised by major features of hyperextensibility skin, atrophic scars and generalised joint hypermobility (GJH); minor features include soft, doughy skin, easy bruising, musculoskeletal pain, and family history[1-3]. With a prevalence of 1:20,000, about 90% of cases of cEDS are caused by mutations in type V collagen, a minor fibrillar collagen with a wide tissue distribution[1,3].
n cEDS, the type V collagen has mutations of the COL5A1 and COL5A2 alleles, which contributes to a haploinsufficiency[1,3]. The clinical diagnosis can be challenging, especially when symptoms overlap with other EDS subtypes or other CTDs. Therefore, a definitive diagnosis of cEDS relies on genetic studies[1-7].
Arterial dissections have been reported previously as a rare finding in cEDS patients[3,5]. Here, we report a young female woman presenting with a distal aortic dissection, whose diagnosis of cEDS was made along with a finding of a novel frameshift mutation in the COL5A1 allele.
CASE DESCRIPTION
A 39-year-old Caucasian female was referred to our outpatient unit with a 10-year history of back and bilateral hip pain, chronic easy bruising, episodes of palpitations, dizziness, and light-headedness. Due to the COVID-19 pandemic restrictions, and the temporal association with the suspension of her global posture re-education (GPR) plan, she experienced additional pain in both wrists, proximal interphalangeal joints, and her left shoulder.
Three months prior to our appointment she had a respiratory infection, with delayed resolution. Due to this infection, a computed tomography (CT) was carried out, which incidentally revealed a distal aorta artery dissection.
Past medical history included a Senning repair due to transposition of the great arteries at 18 months old, hypertension, asthma, allergic rhinitis, scoliosis, repeated respiratory infections, two pregnancies, and one abortion. Current medication included mirtazapine 15 mg, montelukast 10 mg, lisinopril 2.5 mg. No use of tobacco, alcohol, or streets drugs was reported.
Physical examination revealed a body height of 167 cm, joint hypermobility, with a Beighton score of four out of nine, bilateral acromioclavicular joint area tenderness, an atrophic cardiac surgery chest scar, and a systolic murmur – previously known. Based on patient history and clinical findings, a diagnosis of joint hypermobility syndrome was made as per the Brighton criteria.
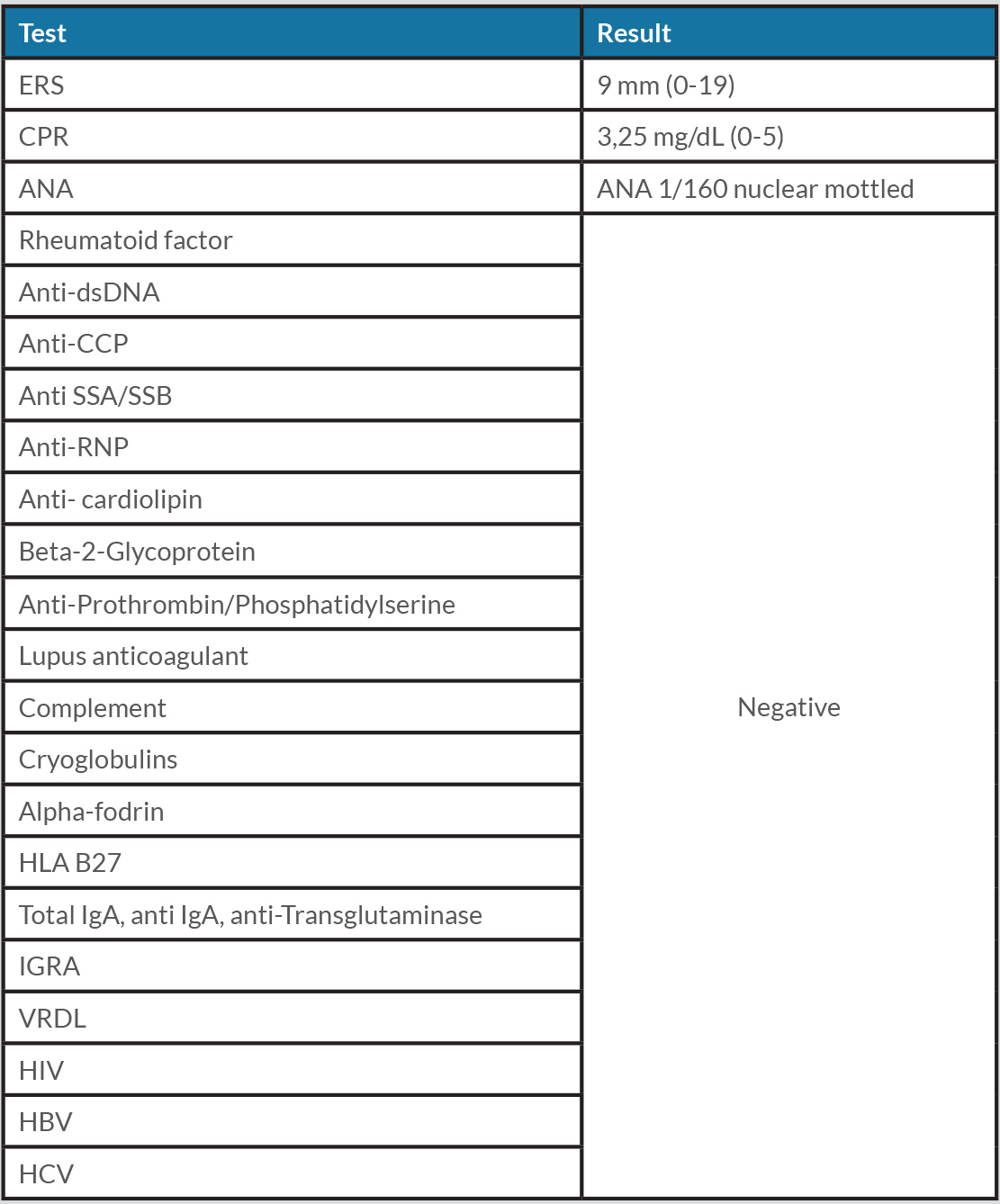
An electrocardiogram showed findings of right ventricular hypertrophy with overload pattern; an echocardiogram revealed Senning’s procedure post-surgical findings and normal left ventricular function. Complete blood count showed a mild thrombocytopenia (127,000/mL). Coagulation tests were unremarkable, as was the extensive immunology workup (Table 1).
Axial CT showed no signs of inflammatory spondyloarthropathy, and MRI excluded sacroiliitis. Thoracic and abdominal CT angiography revealed distal aortic dissection extended through the left common iliac artery.
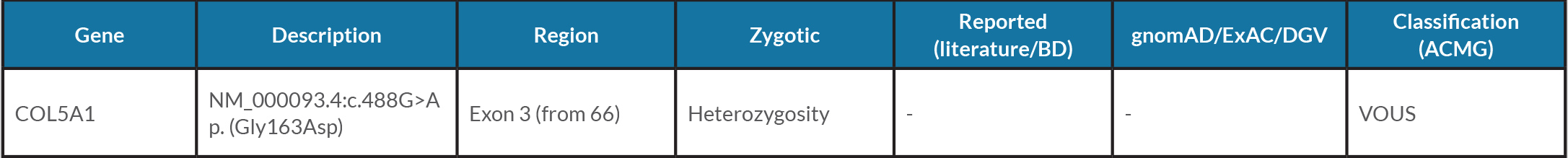
Next-generation sequencing (NGS) using whole-exome sequencing (WES) Marfan-like disorders from 07-2020 (NGS panel based on WES of 77 genes, including analysis of copy number variation from Ehlers-Danlos, Marfan and Loeys-Dietz syndromes, aortic aneurysm, and differential diagnosis) identified a novel frameshift mutation COL5A1 NM_000093.4:c.488G>A p. (Gly163Asp) (Table 2).
In sequence, both parents and her daughter also had genetic studies. Her mother carried the same mutation.
DISCUSSION
EDS represents a heterogeneous group of diseases similar to each other and to other CTDs. Therefore, the cEDS clinical diagnosis can be challenging, even though its major features – GJH, skin hyperextensibility, atrophic scarring, and minor features, easy bruising and pain are well described in literature[1-3]. All those features are present in our patient, whose medical history comprises Senning repair due to transposition of the great arteries at an early age and incidental finding of distal aortic and left common iliac dissection. This led to a genetic study that made a cEDS diagnosis with a never-described variant COL5A1 NM_000093.4:c.488G>A p. (Gly163Asp) according to the Online Mendelian Inheritance in Man (OMIM).
Arterial dissection is rare in cEDS[3,4]. Although it may occur, it is more frequently seen in vascular EDS (vEDS), and in other CTDs such as Marfan syndrome, Loeys-Dietz syndrome, and even in other diseases defined by the aortic aneurism/dissection mutation[5]. For this reason, a genetic study must be conducted to clarify the differential diagnosis.
The new COL51A variant found in our genetic study, although presenting as a missense variant, which are very infrequent in Genome Aggregation (gnomAD) databases, still cannot be totally excluded as a pathogenic variant. Thus, reports of the existence of COL51A variants in related individuals have been described before[3,6], as we found in here. But despite these reports, there is only one case reported in the literature with transposition of the great arteries (TGA) and vEDs, of a female who underwent surgical repair[7] at 16 months old.
The presence of cEDS together with aortic dissection adds more complexity in our case. Because the patient was born with a serious congenital vascular disease, it is tempting to think that both vascular disturbances are part of the same problem and originate from the new COL5A1 variant, through an altered biomechanical property of arterial walls that predisposed spontaneous dissection. Either this is a coincidence or it is not; time will tell if more cases of co-existing transposition of the great vessels and EDS are diagnosed and reported.
The patient was instructed to maintain her GPR plan, and to restrict contact sports. Secondary causes of thrombocytopenia were negative. Strict control of cardiovascular risk factors will be encouraged.
CONCLUSION
This reported case reminds us that even though major features of cEDS are present, vascular fragility must be considered as a rare complication. Genetic factors may influence on the variability of EDS phenotypes as demonstrated by our identification of a novel frameshift mutation in COL5A1 in a patient with cEDS, and aortic dissection. Therefore, when making a cEDS diagnosis, clinicians are reminded that current surveillance may include vascular imaging upon clinical suspicions of vascular involvement.