ABSTRACT
This is a report of a patient who presented with iliofemoral deep vein thrombosis, and was treated with pharmaco-invasive and pharmaco- mechanic methods using coronary balloon and mechanical disruption of clots with coronary 014 wire.
A 65-year-old male presented with acute deep vein thrombosis extending from the left common iliac to the popliteal vein. The patient had signi cant swelling and pain. An inferior vena cava (IVC) lter was inserted, and catheter-directed thrombolysis was planned. A technical dif culty was encountered entering the proximal common iliac vein. Hence, a 014 balance middle weight (BMW) wire with coronary balloon support was introduced through a Cordis® 6 F. diagnostic catheter, and the 014 wire was advanced with guitaring technique up to the femoral vein. Thereafter, the coronary balloon was ruptured at high pressure, and thrombolysis using streptokinase was performed along the balloon tract up to the ostium of the common iliac vein. The patient symptomatically improved signi cantly and is currently on anticoagulants. Follow-up after one year showed minimal residual oedema, and less pain in the ankle region.
Pharmaco-mechanical treatment is possible using coronary balloon dilatations and thrombolysis through a ruptured coronary balloon. Mechanical disruption of clots to some extent is feasible using 014 wire by a guitaring technique.
LEARNING POINTS
- In difficult cases with deep vein thrombosis, coronary hardware could be used for balloon angioplasty, especially when the iliac bifurcation cannot be crossed.
- Even suboptimal results can lead to signi cant symptomatic improvement in deep venous thrombosis treatment.
KEYWORDS
Deep vein thrombosis, IVC lter, catheter-directed thrombolysis
BACKGROUND
Deep vein thrombosis (DVT) is common in clinical practice[1]. The annual incidence of venous thrombosis is 1/1000 adults, and the rates increase sharply after 45 years [2]. Acute iliofemoral thrombosis is associated with signi cant symptoms and with pulmonary embolism features[3]. Around 20% to 50% of patients develop post-thrombotic syndrome, and 5% to 10% of patients develop venous ulcers[4,5]. Hence, adequate acute management is essential in this condition for long-term symptom reduction.
CASE DESCRIPTION
A 65-year-old Asian male presented with oedema in the left lower limb for three days associated with pain in the entire left lower limb. There was no shortness of breath and oxygen saturation at admission was 98% from blood gas analysis. This was the rst episode and he had recently recovered from moderate COVID-19 illness, 15 days before this presentation. He had breathlessness during the symptoms and a plain CT of the chest showed in ltrates with a COVID-19 reporting and data system (CO-RADS) score of 18/25 during the recent illness. He was on oxygen support for a few days for COVID-19 treatment outside the hospital. He has had mild diabetes for 12 years, and has well- controlled hypertension. There was no shortness of breath and recent blood investigations revealed normal creatinine values (0.8 mg/dl). His haemogram showed mild anaemia with a haemoglobin of 10.9 mg/dl. In the past he had varicose veins in the left limb with perforator incompetency, and he was operated on in 2013. He continued to have mild oedema, discoloration, and small venous ulcers in the right lower limb.
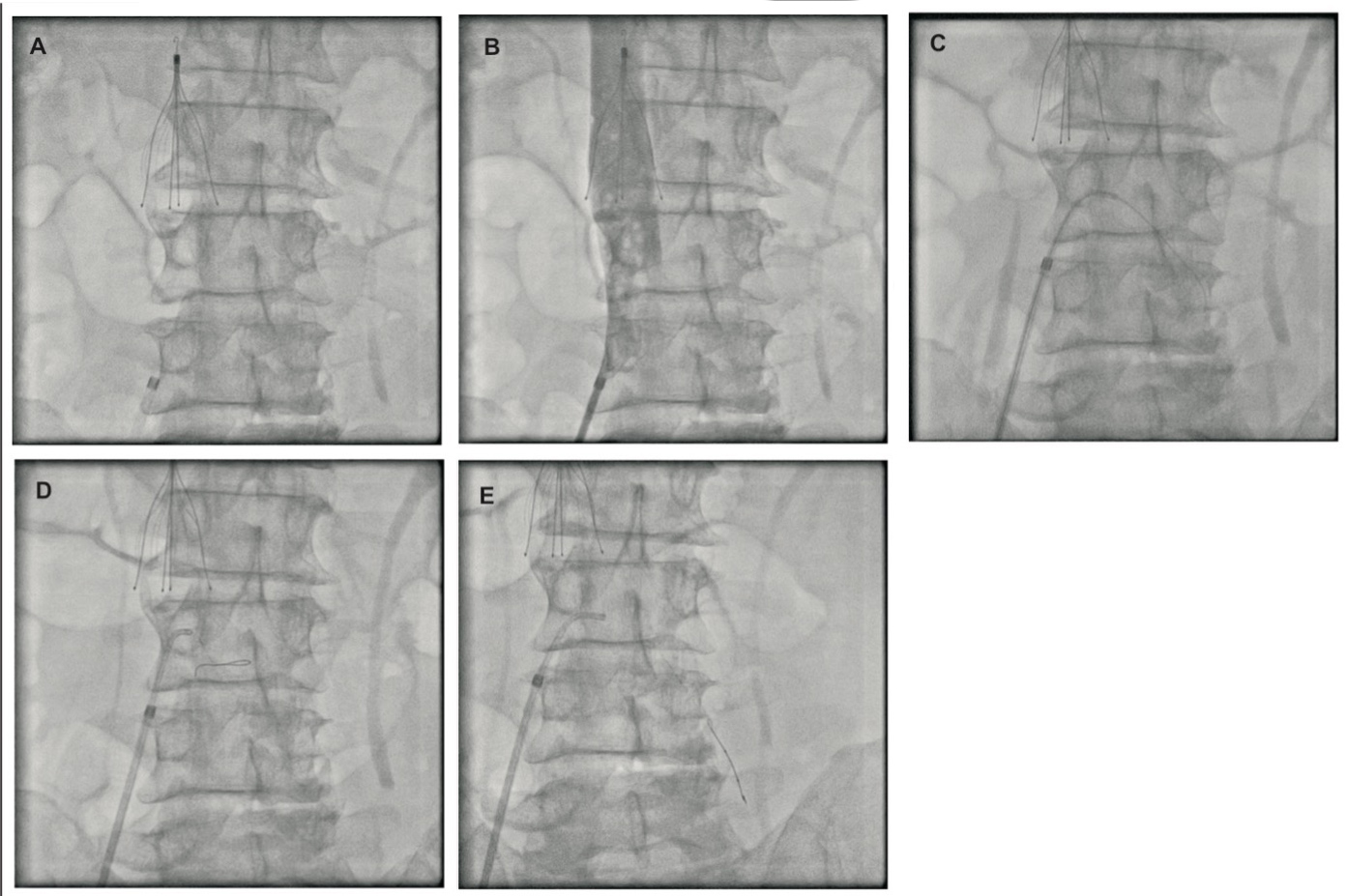
Venous doppler of the limb showed iliofemoral thrombosis extending to the popliteal veins, which was the rst episode. Recent routine blood tests were normal, and the patient had recovered from COVID-19 three weeks before this admission. His investigations at this current admission revealed normal antinuclear antibodies (ANA) and rheumatoid arthritis (RA) factors. The abdomen ultrasound, electrocardiogram, echocardiography, and chest X-ray were also normal. Since the patient had signi cant symptoms, target lesion thrombolysis was planned. First, an inferior vena cava (IVC) filter (Cook Celect TM) was inserted below the renal veins through the right femoral approach (Fig.1A). Clots were observed in the distal end of the inferior vena cava (Fig.1B). Initially, the Cordis 6 F. right coronary artery (RCA) guide catheter was placed at the IVC-common iliac vein junction, and the catheter was advanced to the iliac vein over the tip of 035 hydrophilic wire, but failed. After repeated manoeuvring with Cordis 6 F. right diagnostic catheters and trying to advance Terumo hydrophilic 035 wires and stiff 035 wires (Fig.1C and D), the proximal areas of the left common iliac vein could not be entered or crossed. Hence, 014 balance middle weight (BMW) wire was chosen and it was advanced in the left common iliac veins with 1.5 x 10 mm sprinter balloon support through the Cordis 6 F. diagnostic catheter (Fig.1E). When resistance was encountered during the passage of the wire, a loop was made inside the iliac vein with the BMW wire and it was further advanced using the guitaring technique. The wire was advanced up to the super cial femoral vein. The 014 wire could not be advanced further across the femoral vein due to the hard nature of the clots. Initially, the coronary balloon was advanced and dilatations were given along the tract.
Panel A: IVC lter placement. Panel B: angiogram shows clots in distal IVC-common iliac vein junction. Panel C: 035 dif culty in crossing common iliac vein ostium. Panel D: buckling of 014 wire at the ostium of common iliac vein. Panel E: advancement of 014 wire with coronary balloon support in the common iliac vein.
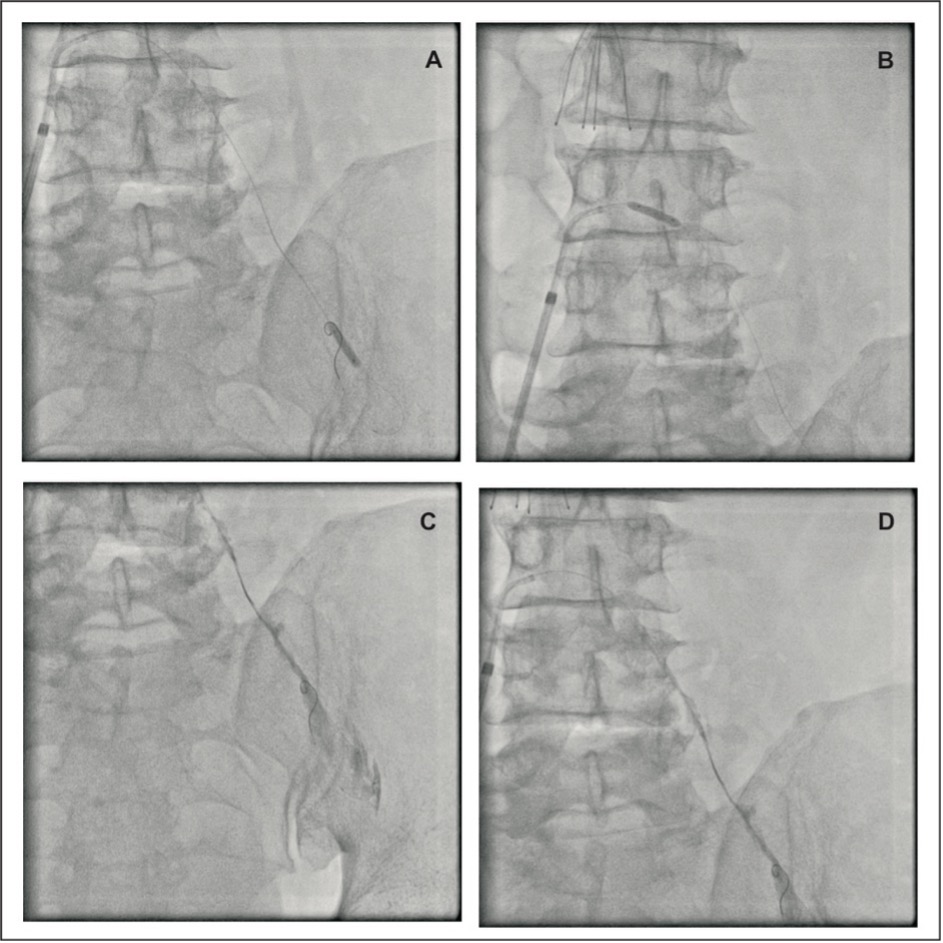
Guitaring was done using the 014 wire with small and larger loops. The smaller 1.5 x 10 mm balloon was then exchanged with a 2.5 x 12 mm coronary balloon (RyureiTM) and serial dilatations at higher pressures were given until the balloon reached the femoral vein (Fig.2A and B). Near the junction of the IVC and the common iliac vein balloon, dilatation was given. Near the femoral vein using higher pressure (28 atm) the coronary balloon was ruptured (Fig.2C), and through the ruptured balloon thrombolysis was performed using streptokinase. Further guitaring movements were performed in that region. Streptokinase 0.75 M units were diluted in 50 ml of normal saline, and slow boluses were given along the path from the origin of femoral vein to the common iliac vein, including the IVC-common iliac veins bifurcation (Fig.2D). A bolus of 15 ml of tiro ban was also given.
Figure 2 Panel A: Balloon dilatation near the femoral vein. Panel B: Balloon dilatation in proximal common iliac vein. Panel C: Balloon rupture at high pressure in common iliac vein. Panel D: Thrombolysis through the ruptured balloon along the tract using streptokinase.
Thereafter, the femoral 6 F. sheath and the 6 F. diagnostic catheter were removed. Post-procedure the patient had shivering, which was reduced with paracetamol injections. Twenty-four hours later, the limb oedema reduced and softness was observed in the thigh, sacro- coccygeal, and gluteal regions, and pain was also reduced (visual analogue scale <50%) in these areas. For the next three days enoxaparin 60 mg SC BD, and clopidogrel 75 mg OD was given. The patient was discharged with clopidogrel 75 mg OD, and rivaroxaban 20 mg OD three days later with further improvement in symptoms.
One month later, the clopidogrel was changed to an alternate-day dose and rivaroxaban 20 mg/day was continued. The three-month follow-up showed reduced limb oedema and minimal swelling below the knee, with mild pain and swelling around the ankle and foot region only. There were no excoriations or impending foot ulcers. The patient is comfortable, without pain, and mild oedema in the foot was seen predominantly in dependent positions and decreases by mild limb elevation during sleep. Ten months post procedure, the patient was having pain in the left lower limb around the left calf region, and rivaroxaban was changed to warfarin. His pain subsided and currently the international normalised ratio (INR) is maintained at around 2. At the one-year follow-up, he had insigni cant pedal oedema, and occasional mild pain around the ankle region.
DISCUSSION
Systemic thrombolysis is associated with lower ef cacy, and an increased risk of major bleeding manifestations[5]. For catheter-directed thrombolysis, various options are available[6-8] and this method is useful and effective in the dislodgement of clots and reducing symptoms[9]. Balloon maceration, balloon venous angioplasty, rheolytic thrombolysis with AngioJetTM, isolated thrombolysis with Trellis, large-bore catheter aspiration are some of the common techniques used in pharmaco-invasive treatment of DVT[10]. In May-Thurner syndrome, endovascular stents are commonly placed in the left common iliac vein[11], and in some non-May-Thurner cases also, which are not associated with adequate results[10,12]. However, the rst step in iliofemoral thrombosis in the right or left side is to cross the occluded proximal or ostial common iliac vein. Technical dif culty is often encountered in crossing the origin or proximal areas of the closed common iliac vein in cases with acute DVT. Hence, in this case with 014 coronary wire and balloon support together with the guitaring technique, the 014 wire can be advanced in the common iliac vein with a heavy clot burden.
In this case, the Cordis 6 F. right diagnostic was used to provide better support for the wire and balloon to cross than guide catheters. The symptoms were signi cantly reduced even though the results were suboptimal. In venous occlusions, suboptimal results can also provide signi cant symptom relief. The streptokinase dose used for direct thrombolysis was 750 000U, which is 50% of the dose used in acute myocardial infarctions. This was because of the anticipated high risk of clotting over indwelling thrombolysis catheter in the opposite limb in the post-COVID-19 scenario of the patient[13]. In this case a smaller balloon was used, but higher-calibre balloons such as 4.5 mm (AccuforceTM, Terumo) or 5 mm balloons (Quantum ApexTM, Boston Scientific) can be taken inside the right coronary 6 F. Cordis diagnostic catheter after balloon maceration and deflation. Thrombolysis using low dose of thrombolytics is useful and usually given as continuous infusion over few days[14]. However, in this case streptokinase was given as a slow bolus over a period of 30 minutes only, through a ruptured coronary balloon along the tract. In this case throughout, only coronary wires and balloons were used; peripheral 035 wires were not used. The guitaring technique has been shown to be useful for mechanical dislodgement of clots in the femoral vessels, using 035 Terumo hydrophilic wire[15]. In this case, the dislodgement of a clot was made using 014 BMW wire using the guitaring technique and thrombolysis was performed using a punctured balloon. It is preferable to insert an IVC lter prior to the procedure, since during thrombolysis the possibility of dislodgement of the clots is high, which could lead to pulmonary embolism during thrombolysis[16].
Some centres do not use IVC lters during catheter-directed thrombolysis or AngioJet; they usually insert them only if clots are seen in the inferior vena cava. In this case, clots were visualised in the inferior vena cava–iliac vein junction. Coronary balloons are available in all catheterisation labs, and the need for specialised suction and aspiration[17] or thrombolysis catheters such as AngioJet[18] are not required – most of these are available only in major tertiary care centres. Hence, this technique can be performed in any interventional cardiac or vascular lab.
AngioJet is increasingly used nowadays for venous thromboembolism. It is a valuable technique, and the approach has to be through the ipsilateral popliteal vein. Since the AngioJet catheters for venous aspirations are 8F, the contralateral approach is dif cult technique-wise; hence the ipsilateral process is the current method for DVT using AngioJet. Also, locating the popliteal vein and venous cannulation in the occluded popliteal vein through doppler visualisation is often challenging.
CONCLUSION
Catheter-directed thrombolysis is useful in the treatment of DVT; suboptimal results during thrombolysis in DVT treatment is also useful. Technical dif culty is frequently encountered in crossing the proximal common iliac vein in iliofemoral thrombosis. Using a 014 wire with guitaring movement on a coronary balloon support is a good method to reduce iliofemoral DVT symptoms. Coronary balloons can be used in the treatment of iliofemoral DVT for balloon dilatation and thrombolysis through the ruptured coronary balloons.