ABSTRACT
Myomatous erythrocytosis syndrome (MES) is a rare gynaecological condition associated with the presence of a uterine fibroid and isolated polycythaemia. The main characteristic of MES is that haemoglobin returns to a normal level after removal of the myoma. MES is poorly known and still not fully understood. This case report describes the history of a patient with MES with surprising erythrocytosis resolution after myomectomy.
LEARNING POINTS
- A case of myomatous erythrocytosis syndrome with a normal erythropoietin level is described, adding to the scarce literature; the mediator responsible for the erythrocytosis is not yet known.
- This is a rare presentation of a common condition: erythrocytosis and uterine fibroids are frequent in the general population but are only anecdotally correlated.
- Delayed diagnosis led to unnecessary aggressive treatment with the aim of reducing the haematocrit level to below 45%.
KEYWORDS
Erythrocytosis, polyglobulia, leiomyoma, myomatous erythrocytosis syndrome, MES
INTRODUCTION
Myomatous erythrocytosis syndrome (MES) is a rare cause of secondary polycythaemia linked to the presence of a uterine fibroid. We report the fortuitous discovery of non-symptomatic polycythaemia in a 34-year-old patient without relevant comorbidities.
CASE DESCRIPTION
A 34-year-old woman presented with isolated polycythaemia incidentally discovered on a routine blood test 10 months post-partum. The patient was not on any treatment, did not use tobacco and did not have any symptoms consistent with chronic hypoxaemia. There were no significant comorbidities, with the exception of an asymptomatic uterine fibroid.
Since her third pregnancy, the patient has been followed by gynaecologists for this asymptomatic and subserosal uterine fibroid; the last ultrasound follow-up showed a stable larger diameter of 8 cm. Concurrently, the patient was diagnosed with isolated asymptomatic erythrocytosis with a haemoglobin level of 19.9 g/dl (normal value (NV) 12–16 g/dl) and a high haematocrit level of 60.5% (NV 35–47), while platelet and leukocyte counts were normal.
Physical examination was completely normal, with the exception of mild bilateral conjunctival erythema. Oxygen saturation was 98% on room air. The blood erythropoietin (EPO) level was normal at 5.7 U/l (NV 4.3–29). Abdominal ultrasound did not show hepatomegaly or splenomegaly, with no renal lesions or Doppler evidence of abnormal renal perfusion. The presence of a large, lateralized, 12 cm-long uterine myoma on the left side was confirmed. Polycythaemia vera (PV) was first suspected and, while awaiting the baseline medullary work-up results, the patient underwent anti-aggregant therapy with aspirin 80 mg once daily and four phlebotomies aimed at lowering the haematocrit level to below 45%.
A complete medullary assessment to confirm primary polycythaemia[1] was carried out. The bone marrow histology was not in favour of a primary myeloproliferative neoplasm, the karyotype was a normal female karyotype in 20 out of 20 metaphases, and the NGS evaluation for JAK2 V617F, exon 12, CALR and MPL mutation was negative. PCR evaluation for exon 7 and 8 mutations of the EPO-receptor was also negative.
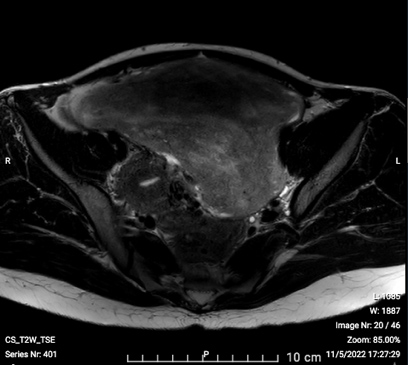
The patient was then suspected of having MES. On clinical examination, her uterus was the size of that of a woman at 20 weeks of pregnancy. The abdominal and pelvic MRI showed the presence of a bulky heterogeneous mass measuring approximately 17.4×9.0×17.2 cm with an intermediate signal on T2 weighting (Fig. 1). A myomectomy was advised and was performed by laparotomy in June 2022. The surgical specimen weighed 1410 g and measured 19×14×10 cm. The pathology was in favour of a uterine leiomyoma without signs of malignancy. There were no complications in the postoperative period and no further treatment was needed.
In the postoperative period, the haemoglobin level dropped to 12.5 g/dl and remained stable over the next months without additional phlebotomies. The patient was thus diagnosed as having MES and cured with the removal of the fibroid.
DISCUSSION
MES is a rare cause of isolated secondary polycythaemia with about 50 cases described so far. The first case was published in 1953 by Thomsen and Marson[2].
Our case fulfils the three diagnostic criteria proposed by Fleming and Markley: (i) polycythaemia, (ii) uterine myoma and (iii) restoration of a normal haemoglobin level after surgical removal of the fibroid[3].
The pathophysiological mechanism of MES remains incompletely understood. Several hypotheses have been proposed, the most probable at present being the autonomous synthesis of EPO by the fibroid without negative feedback, first hypothesized in 1963 by Hertko[4]. In 1999, the presence of EPO-specific immunostaining was demonstrated in the cytoplasm of uterine leiomyoma cells from a patient with MES[5]. More recently, EPO-receptor levels were found to be increased in the endothelial cells of a fibroid in a patient with MES, suggesting the hypothesis of a possible link between the large size of the fibroids found in MES and the EPO/EPO-receptor system[6,7].
Despite its certain role in the pathophysiology of MES, EPO blood level is not a reliable indicator of the disease. Although most cases of MES have an increased blood EPO level, very few cases of MES with a normal EPO level have been reported in the literature[5,8]. As described in our patient, a normal EPO level can make the diagnosis of secondary polycythaemia more difficult.
MES remains a rare cause of secondary polycythaemia and requires the intervention of a multidisciplinary team in order to make the diagnosis. The rarity of this entity poses a diagnostic challenge for many internists and haematologists, resulting in the risk of delayed diagnosis, misdiagnosis and inappropriate treatment.