ABSTRACT
Cryptococcosis is an opportunistic fungal infection seen in immunocompromised individuals. It is caused by the yeast-like fungus Cryptococcus and predominantly affects the lungs and central nervous system. Immunocompetent individuals very rarely develop bone involvement and only a few cases of cryptococcal osteomyelitis in patients without other comorbid conditions have been described. Only one other case of pelvic involvement, which was accompanied by lymphopaenia, has been reported. We describe the case of a 42-year-old immunocompetent man with cryptococcal hip osteomyelitis.
LEARNING POINTS
- Osteomyelitis due to Cryptococcus is very rare.
- Cryptococcal osteomyelitis is uncommon in immunocompetent individuals.
- Prompt intravenous treatment with antifungal medication should be offered to all patients with cryptococcal osteomyelitis.
KEYWORDS
Cryptococcus, cryptococcosis, cryptococcal osteomyelitis, immunocompetent
CASE DESCRIPTION
A 42-year-old middle-class male solar power plant worker started to experience poorly localized low backache. He was from southern India and newly diagnosed with type 2 diabetes mellitus (HbA1c 6.8). He presented to a nearby physiotherapy clinic with intermittent pain and discomfort and received short wave diathermy and transcutaneous electrical nerve stimulation (TENS) on three separate occasions over 1 month with no relief of symptoms. The pain started to radiate down the left posterior thigh and leg and intensified after 15 days, when the patient began to have trouble walking. Over the next 5 days he experienced nocturnal fever, which led him to seek medical advice. There was no history of weight loss, difficulty breathing, bowel or bladder disturbance, intravenous drug use or high-risk sexual behaviour.
On examination, the patient was well built and well-nourished with a BMI of 22.3 kg/m2. His vital signs including temperature, pulse rate, blood pressure, oxygen saturation and respiratory rate were within normal limits. Lymph node examination was unremarkable. Other systemic examinations were also unremarkable. Laboratory work-up showed nothing significant.
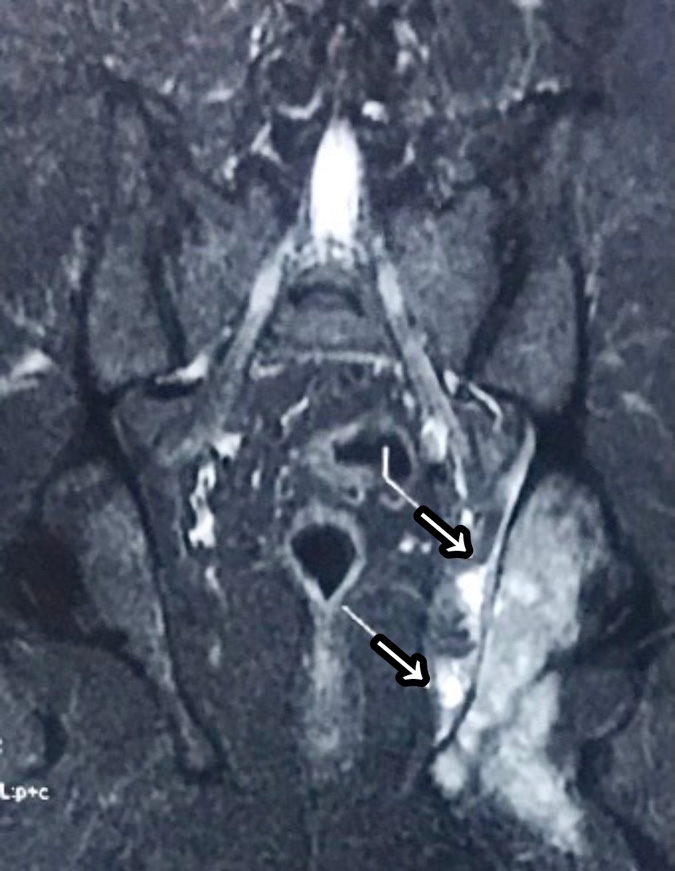
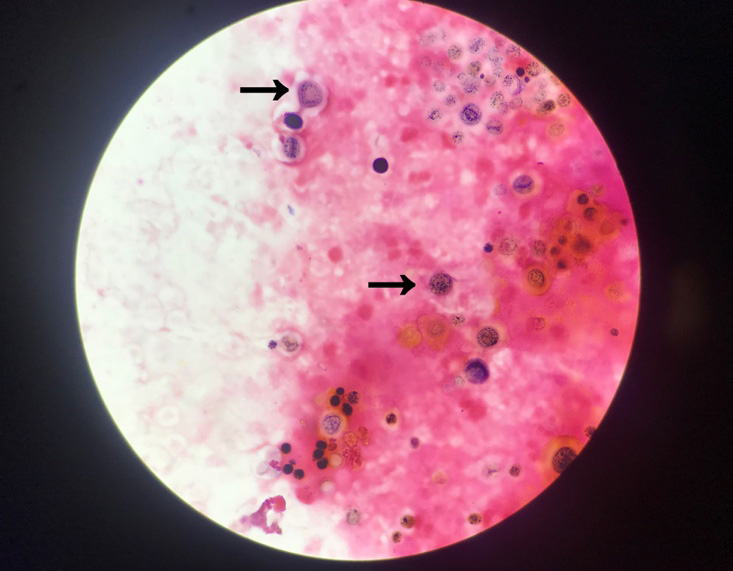
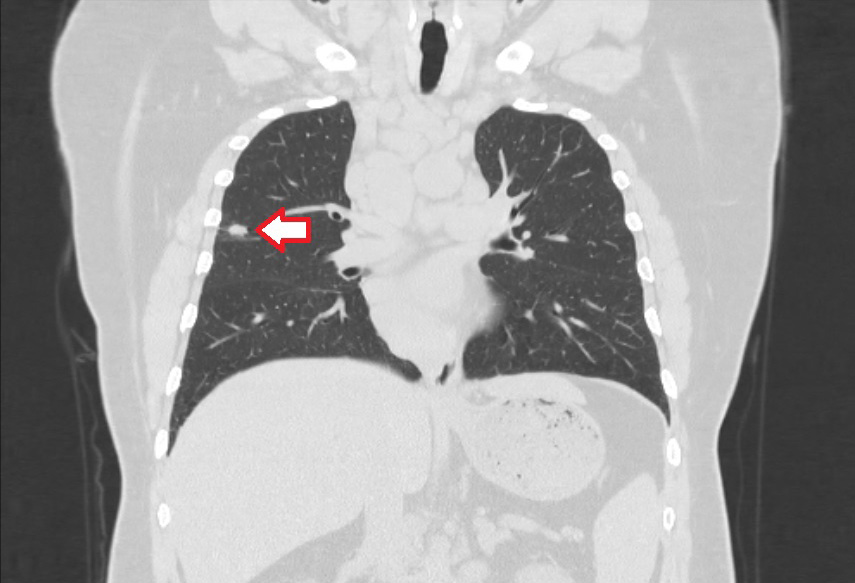
The patient was advised to undergo magnetic resonance imaging (MRI) because of the prolonged pain. MRI of the hip revealed hyper-intense areas in the left ischial tuberosity and inferior pubic ramus on STIR, and soft tissue oedema involving the pyriformis, external and internal obturator muscles, suggestive of osteomyelitis of the left ischial tuberosity (Fig. 1). The patient subsequently underwent computed tomography (CT)-guided biopsy of the left ischium bone. The sample was sent for culture and sensitivity testing. The nucleic acid amplification test (NAAT) for tuberculosis and resistance to rifampicin assay (RIF) were negative. Microscopic examination of the biopsy sample revealed “non-viable bone spicules with focal necrosis, ill-defined granulomas & exudative inflammation with Cryptococcus, consistent with fungal osteomyelitis” (Fig. 2). Tests for HIV, hepatitis B and C were negative. The CD4 T-cell count was 975 cells/μl and the CD8 T-cell count was 967 cells/μl, well within the normal ranges. A serum cryptococcal antigen test was positive. CT of the chest was performed since cryptococcal osteomyelitis is rare in immunocompetent individuals without any pulmonary involvement. CT revealed a 1.2×1.1 cm nodular lesion in the right upper lobe, ill-defined small centrilobular ground-glass nodules in the right lower lobe base, mediastinal adenopathies (some with calcification), and multiple discrete para-aortic, aortocaval and paracaval nodes suggesting the possibility of a granulomatous lesion (Fig. 3).
Figure 1. MRI of the hip suggestive of osteomyelitis of the left ischial tuberosity
Figure 3. CT of the chest showing a right upper lobe nodular lesion (probable granuloma)
The patient was admitted for curettage and debridement of the infected area. Intravenous liposomal amphotericin B and flucytosine were started. He developed acute kidney injury after administration of liposomal amphotericin B, which was managed with antifungal dose reduction. The patient was discharged on intravenous liposomal amphotericin B and flucytosine for 3 weeks, followed by fluconazole 400 mg once daily for 6 months. A month after discharge, the patient is doing well.
DISCUSSION
Previously known as European blastomycosis, torulosis or Busse-Buschke disease, cryptococcosis is an opportunistic infection caused by either Cryptococcus neoformans, typically present in soil contaminated with avian excreta, or Cryptococcus gattii, which is found on trees, especially eucalyptus. After infected aerosolized particles are inhaled, the infection is either cleared or latent infection is established, perhaps in granulomas, with the lungs serving as the principal foci. Disseminated infections frequently involve the central nervous system and osseous lesions are uncommon (5–10%)[1].
It is rare for cryptococcosis to manifest as osteomyelitis of the pelvis. Very few HIV-negative patients have been diagnosed with cryptococcal osteomyelitis. The most common underlying condition in these individuals was sarcoidosis, followed by tuberculosis, steroid treatment, lymphoma and leukaemia[2].
A study of 44 patients aged 3–79 years found cryptococcal osteomyelitis predominantly involved the vertebrae, followed by the ribs/scapula, femur, humerus and skull[3]. A PubMed search using the search terms ‘cryptococcal osteomyelitis’ and ‘immunocompetent host’ yielded 22 results. Only one of these patients had a lesion on the hip[4].
Plain radiographs are the initial step in the radiological assessment of osteomyelitis. However, it takes 10–21 days after infection before a 30–50% decrease in bone density allows an osseous lesion to be seen on conventional radiographs[5]. The radiological findings are non-specific, and lesions typically appear purely lytic, with discrete margins and with or without periosteal reactions. Identification of the microorganism in the bone lesion can provide a conclusive diagnosis.
Cryptococcus species in CSF and other body fluids can be quickly and cheaply identified using India ink microscopy. Light microscopy may be used to observe the stain’s halo of light that forms when it covers the background field but is not absorbed by the thick polysaccharide capsule of Cryptococcus. Other staining techniques include Fontana-Masson stain (identifies melanin in the yeast cell wall) and Grocott-Gomori methenamine silver stain[6–8].
According to the Infectious Diseases Society of America, treatment consists of intravenous liposomal amphotericin B 3–4 mg/kg once daily plus oral flucytosine 25 mg/kg four times a day for 2 weeks, followed by consolidation therapy with oral fluconazole 400–800 mg once daily for 8 weeks. Maintenance therapy consists of oral fluconazole 200 mg once daily for 1 year or more from the initiation of antifungal therapy[9].
In conclusion, the possibility of cryptococcal infection in a immunocompetent individual with skeletal involvement must be borne in mind despite being rare. Morbidity and mortality can be reduced with prompt diagnosis and appropriate intervention.