ABSTRACT
Introduction: We describe a case of remitting seronegative symmetrical synovitis with pitting oedema (RS3PE) syndrome following administration of the ChAdOx1-S/nCoV-19 [recombinant] vaccine, suggesting a possible causal link.
Case Description: A 72-year-old man presented to his general practitioner with swollen, oedematous hands and legs 2 weeks after receiving a coronavirus vaccine. He had raised inflammatory markers but remained systemically well. He was initially presumed to have cellulitis, but his symptoms persisted despite several courses of antibiotics. Deep vein thromboses, cardiac failure, renal failure and hypoalbuminaemia were ruled out. Upon Rheumatology review, he was diagnosed as having RS3PE syndrome with the Covid vaccine suspected of being an immunogenic trigger. Following initiation of steroid therapy, his symptoms improved dramatically, as is characteristic of RS3PE syndrome.
Discussion: The pathophysiology of RS3PE is unclear. It is known to have various triggers and associations including infections, certain vaccines and malignancy. This case highlights that a coronavirus vaccine (ChAdOx1-S/nCoV-19 [recombinant] vaccine) is also a possible trigger. Factors that make the diagnosis likely include an acute onset of symptoms including pitting oedema in a typical distribution, age above 50, and unremarkable autoimmune serology. Other learning points from this case include the importance of antibiotic stewardship and the need to explore non-infectious causes of illness when antibiotics do not improve symptoms.
Conclusion: The ChAdOx1-S/nCoV-19 [recombinant] vaccine is a possible trigger of RS3PE. However, the benefits of vaccines against coronavirus outweigh the risks in the majority of patients.
LEARNING POINTS
- This case demonstrates a possible link between the ChAdOx1-S/nCoV-19 [recombinant] vaccine and autoimmune conditions such as RS3PE.
- It is important to consider alternative diagnoses when antibiotic regimes fail to work.
- A barrier to accurate diagnosis includes an episodic approach, where a patient presents to multiple clinicians acutely rather than having a long-term, continuous relationship with a single multi-disciplinary team, where response to treatment can be monitored.
KEYWORDS
RS3PE, ChAdOx1-S/nCoV-19 [recombinant] vaccine, coronavirus
CASE DESCRIPTION
A 72-year-old man was referred to the Deep Vein Thrombosis (DVT) Clinic in May 2021 with a few months’ history of an erythematous, painful, swollen right leg and bilateral lower limb peripheral oedema. He also reported arthralgia of his shoulders and hands. The pain in his upper and lower limbs was worse in the mornings, with accompanying joint stiffness that improved with activity. He denied any history of trauma or injury. There were no specific features to suggest giant cell arteritis, including no temporal headache, visual disturbance, or jaw and tongue claudication. He had no significant past medical history. He had received the ChAdOx1-S/nCoV-19 [recombinant] vaccine 2 weeks prior to the onset of his symptoms in February 2021. On clinical examination, he had bilateral lower limb peripheral pitting oedema reaching his knees, with more pronounced swelling in his right leg. There was generalised swelling of his hands, with significant pitting oedema to the dorsal aspect, but no discrete joint swelling. At presentation he had a raised C-reactive protein (CRP) of 138 mg/l with a normal white cell count of 9.9×109/l, neutrophils of 7.02×109/l, and lymphocytes of 1.72×109/l.
An ultrasound Doppler of the right lower leg did not show any deep vein thrombosis (DVT). Pro-beta natriuretic peptide was mildly raised. An echocardiogram confirmed good systolic and diastolic function (left ventricular ejection fraction of 55%), with no significant valvular abnormalities. Although the patient had previously received two courses of antibiotics for this problem from his general practitioner (GP), the hospital team treated it as ongoing cellulitis and prescribed a further course of oral flucloxacillin.
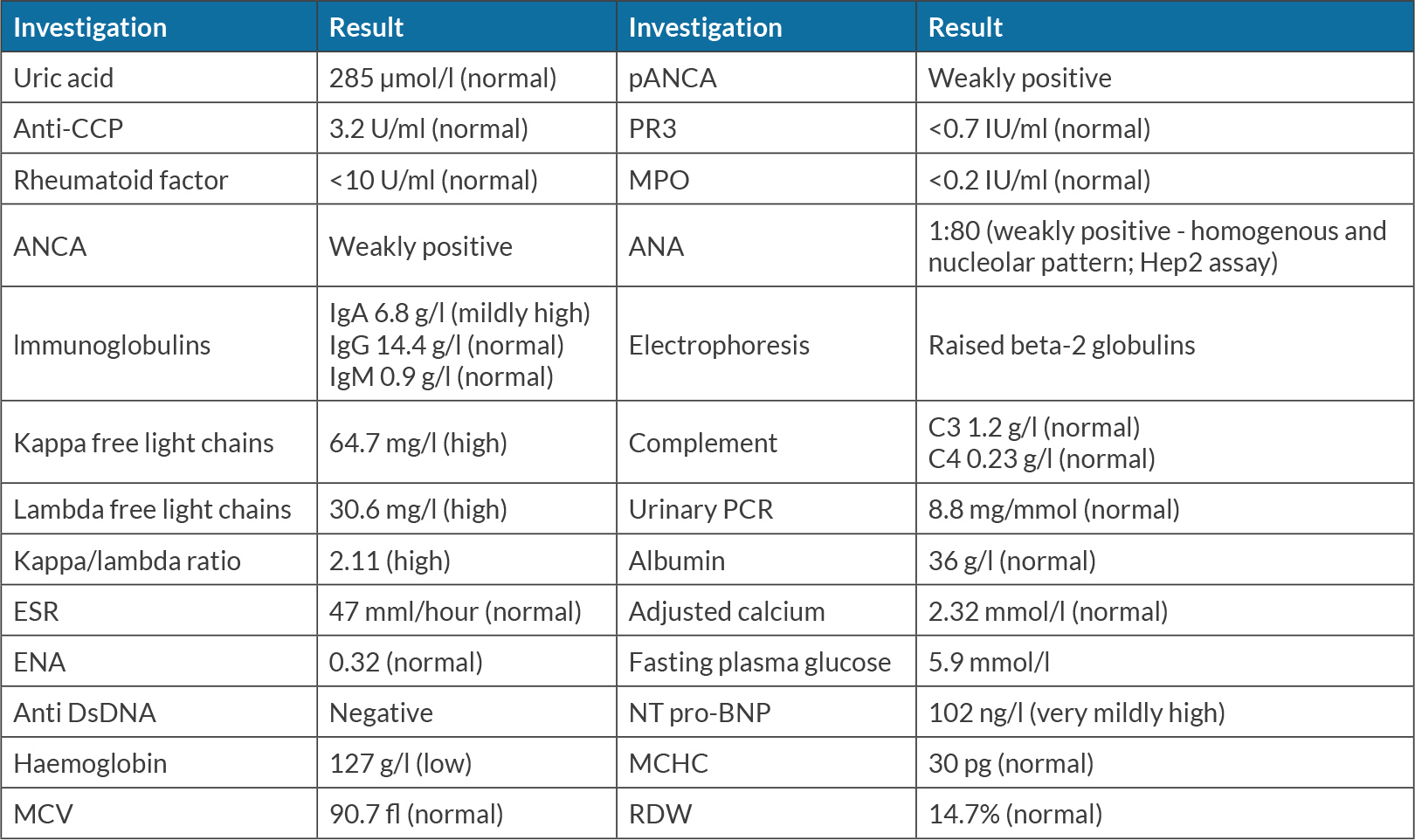
Over the course of the next few months, the patient received further courses of antibiotics with no improvement in his symptoms. Although he remained systemically well, his symptoms and raised inflammatory markers persisted. He was eventually seen by the Infectious Diseases team, who felt cellulitis was unlikely and diagnosed him as likely having chronic venous insufficiency, with advice to wear compression stockings. His GP referred him to the Care of the Elderly department for assessment in October 2021. By this point the pitting oedema in his legs had reached his thighs, with ongoing pitting oedema to his hands. A Rheumatology review was requested with further blood tests (Table 1).
His weakly positive ANA was thought to be clinically insignificant as there were no features of connective tissue disease. Electrophoresis and immunoglobulins were suggestive of monoclonal gammopathy of undetermined significance (MGUS) for which surveillance was planned.
It was felt his presentation was in keeping with remitting seronegative symmetrical synovitis of the hands and pitting oedema (RS3PE). Due to the link between RS3PE and malignancy, a CT of the chest, abdomen and pelvis was organised, which showed no malignancy. A prostate specific antigen (PSA) test was also performed, which was normal. Given the temporal relationship of symptom onset to his Covid vaccine, it was hypothesised this may be implicated. A weaning dose of prednisolone was initiated, with 15 mg once daily for 2 weeks, followed by 10 mg once daily for 2 weeks, and then subsequent reduction by 1 mg every 2 weeks.
Following initiation of steroids, the patient noted a significant reduction in symptoms, and near resolution of the oedema. He continues to do well on subsequent outpatient review. He will remain under monitoring by the Rheumatology team for the time being.
DISCUSSION
The pathophysiology of RS3PE remains unclear. Due to the high levels of serum vascular endothelial growth factor (VEGF) found in previously reported cases of the disease, it is thought that VEGF is implicated in the increased vascular permeability and subsequent peripheral oedema that occurs in RS3PE[1]. The literature also reports increased interleukin-6 levels in patients with RS3PE, consistent with the inflammatory nature of the disease[2]. The exact aetiology remains unknown, although several triggers and associations have been identified. Infections such as parvovirus B-19[3] and tuberculosis[4] have been found in patients presenting with RS3PE, suggesting potential susceptibility of the disease is brought on by infections. RS3PE is also associated with malignancy, presenting as a paraneoplastic polyarthritis syndrome, with up to 54% of patients with RS3PE having some form of malignancy[5].
Symptoms of RS3PE include peripheral pitting oedema in the hands and feet as well as polyarthritis of peripheral joints. At a patient’s initial presentation, the peripheral oedema in their legs may be thought to be thrombo-embolic in nature, but DVTs usually present unilaterally instead of bilaterally. As the condition persists, skin discolouration is brought on by gravity, venous insufficiency and swelling. When associated with raised inflammatory markers, this might prompt clinicians towards a diagnosis of cellulitis, as in our patient. However, factors that help distinguish RS3PE from cellulitis include the involvement of both legs, bilateral cellulitis being a rare entity[6]. Venous insufficiency would also not necessarily explain pitting oedema in the patient’s hands. RS3PE is also associated with polyarthralgia, as in our patient who had pain and stiffness in the shoulders. Differential diagnoses include polymyalgia rheumatica and other inflammatory arthropathies, making the diagnosis of RS3PE a challenging one. Our patient had unremarkable autoimmune serology, an acute onset of the condition, pitting oedema and an age above 50, all of which were suggestive of RS3PE[7]. The diagnosis is further supported by a marked improvement with steroids, as seen in this case.
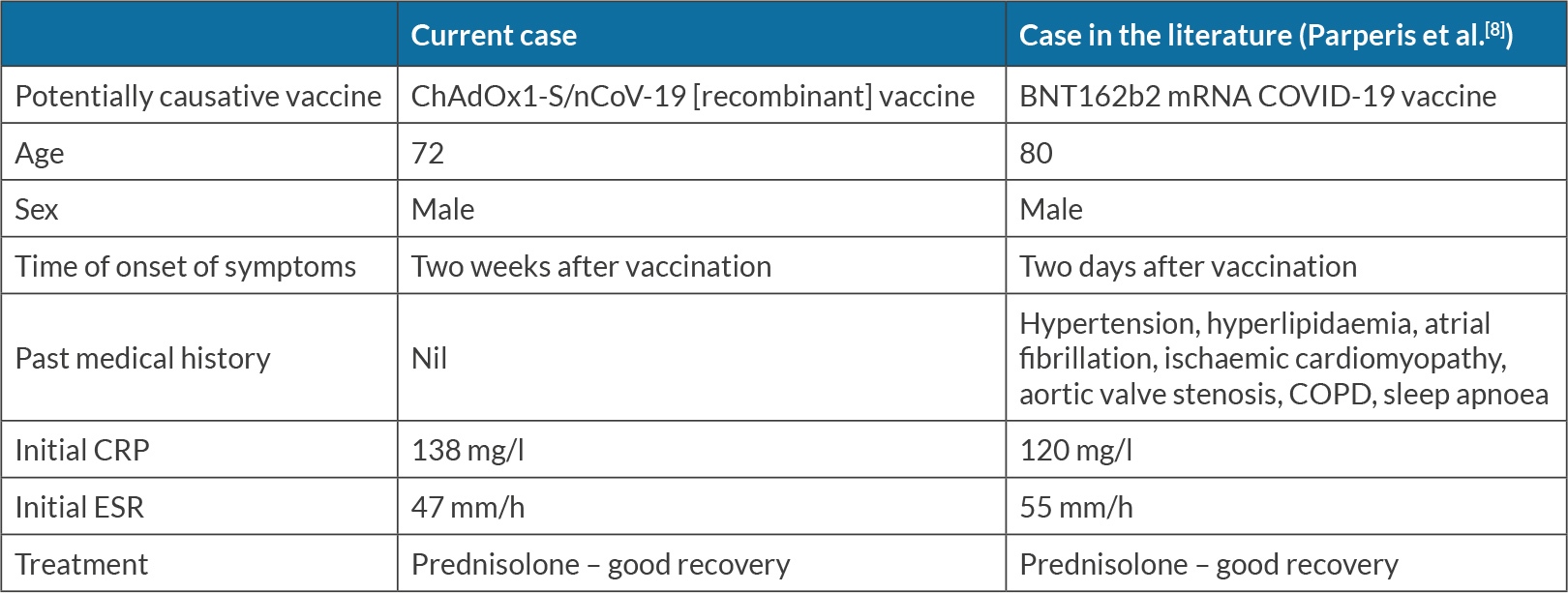
In this case, the patient’s symptoms started shortly after he received the ChAdOx1-S/nCoV-19 [recombinant] vaccine, the temporal relationship suggesting the vaccine was a possible immunogenic trigger. Patients have been reported to develop RS3PE following administration of the BNT162b2 mRNA vaccine[8], but, as far as we know, this is the only reported instance of RS3PE occurring following administration of the ChAdOx1-S/nCoV-19 [recombinant] vaccine. Table 2 outlines several differences between these two cases.
Table 2. Comparison between cases of seronegative symmetrical synovitis with pitting oedema (RS3PE) potentially secondary to Covid vaccination
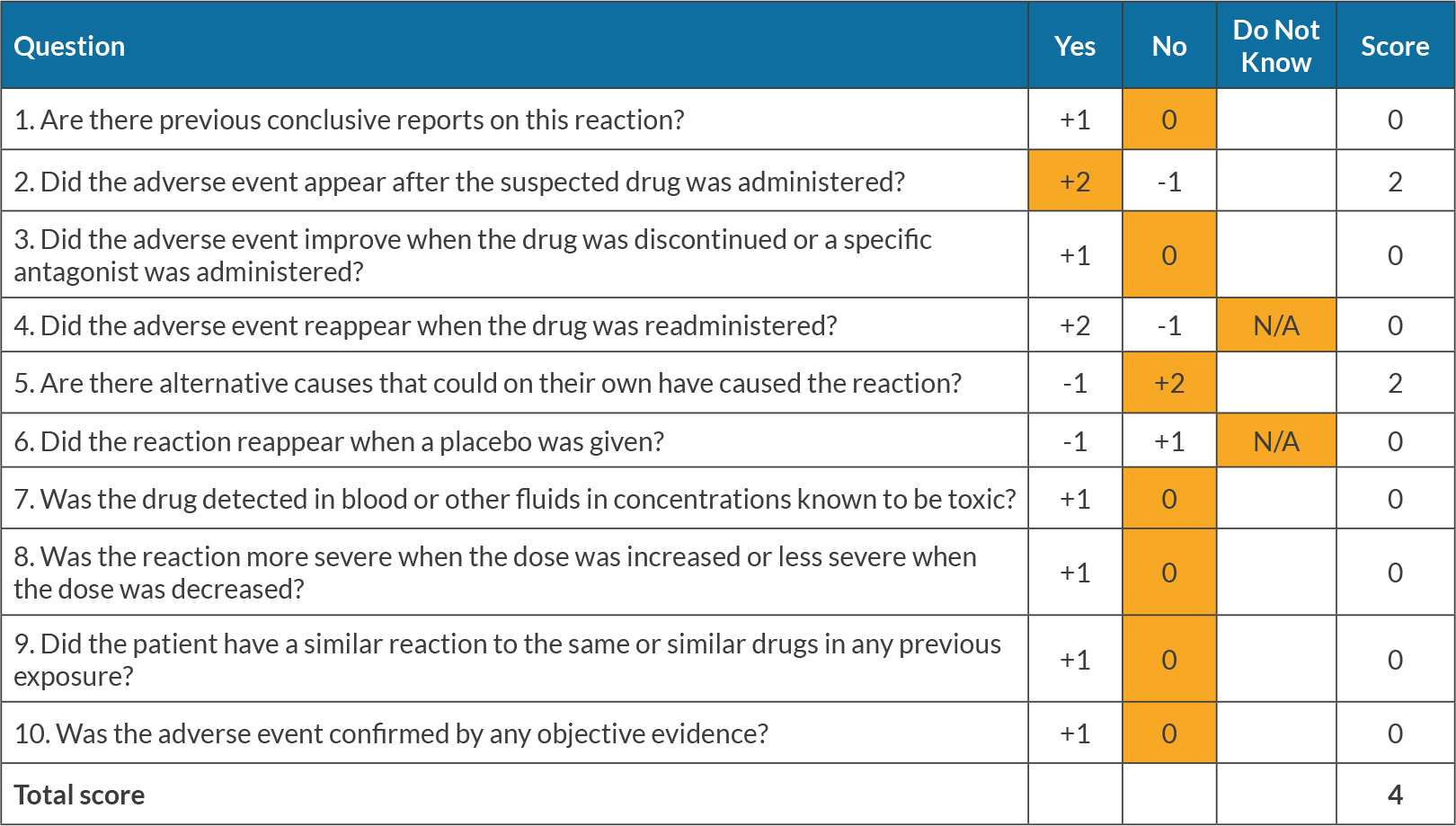
As it is impossible to perform randomised controlled trials to evaluate the strength of the association between Covid vaccines and RS3PE, it is important to highlight such cases in order to better understand these links. The Naranjo score of likelihood of association[9] between the Covid vaccine and RS3PE in this case is 4, indicating that the drug is a ‘possible’ cause of RS3PE. Table 3 outlines the Naranjo score of association in detail. It is important to acknowledge that RS3PE is often secondary to a malignancy, and it is possible that this patient has a malignancy that is yet to manifest itself, although an initial screen has so far been negative.
CONCLUSION
The ChAdOx1-S/nCoV-19 [recombinant] vaccine is a possible trigger for RS3PE syndrome.