ABSTRACT
Introduction: Spontaneous renal haemorrhage is a rare condition with potentially serious complications.
Case description: We describe a 76-year-old woman with a 3-day history of fever and malaise, with no associated trauma. She was admitted to our emergency room with signs of shock. A contrast-enhanced computed tomography scan revealed an extensive right kidney haematoma. Despite fast surgical management, the patient died less than 24 h after admission
Conclusion: Spontaneous renal haemorrhage should be quickly identified due to its fatal complications. Early diagnosis leads to a better prognosis.
LEARNING POINTS
- Spontaneous renal haemorrhage is a severe and rare condition in the absence of trauma and antithrombotic therapy.
- Contrast-enhanced abdominal CT scan is the gold standard for diagnosis.
- Surgical nephrectomy should be considered in haemodynamically unstable patients.
- Conservative therapy with intravenous resuscitation and blood products should be considered in stable patients
KEYWORDS
Spontaneous renal haemorrhage, renal haematoma, Lenk’s triad
INTRODUCTION
Spontaneous renal haemorrhage or haematoma (SRH) is a rare but potentially fatal condition. It consists of intraparenchymal and perirenal haemorrhage in the absence of trauma or antithrombotic therapy. SRH is most frequently described in patients with vascular renal tumours such as renal cell carcinoma and angiomyolipoma, vasculitides or vascular malformations. The classic presentation includes flank pain, with a palpable flank mass and hypovolaemic shock. A contrast-enhanced computed tomography scan is the gold standard for diagnosis. Management options include both surgical and conservative therapy[1]. We present a case of SRH with secondary shock, with an unfavourable outcome.
CASE DESCRIPTION
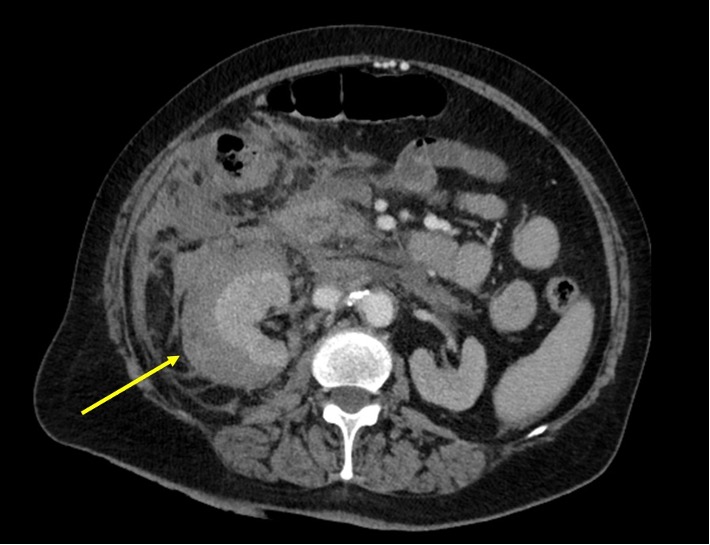
We describe the case of a 76-year-old woman with a 3-day history of fever and malaise. She had been recently diagnosed with epidermoid lung cancer and referred to Oncology for consultation. She also had a history of arterial hypertension, dyslipidaemia, chronic kidney disease KDIGO 3b, and a previous smoking habit. She had no history of antithrombotic drugs or non-steroidal anti-inflammatory drug use. She was admitted to our Emergency Room with signs of sepsis, hypotension, confused conversation (Glasgow Coma Scale 14), fever (39.2ºC) and signs of impaired peripheral perfusion, with mottling. Blood investigations, including arterial blood gas analysis, revealed acute anaemia with Hb 9.0 g/dl, a normal leucocyte count, thrombocytopenia (129×109/l), elevated D-dimers (28.69 µg/ml), a slightly increased prothrombin time (14.7 s) with INR 1.27, a normal thromboplastin time and fibrinogen levels, acute kidney injury with P-creatinine 2.90 mg/dl, elevated C-reactive protein and procalcitonin levels (7.41 mg/dl and 8.50 ng/ml, respectively), anion-gap metabolic acidosis and type A hyperlactacidaemia (80 mg/dl). Due to refractory hypotension, vasopressor therapy with norepinephrine was started, with a slight serum lactate level decrease. Broad-spectrum antibiotic coverage with piperacillin-tazobactam and vancomycin was started. A full-body CT scan revealed an extensive haematoma in the superior pole of the right kidney, that expanded to the remaining retroperitoneum and root of mesentery (Fig. 1). A diagnosis of hypovolaemic shock secondary to SRH was made, and the patient was submitted to right radical nephrectomy. The patient was then admitted to our Intensive Care Unit. However, despite adequate medical and surgical therapy, the patient died less than 24 h after admission.
Figure 1. Contrast-enhanced abdominal CT scan shows a right intraparenchymal and perirenal haematoma. No abnormal vascular malformations or tumours were found
DISCUSSION
SRH is a rare condition in clinical practice and has serious complications. It consists of intraparenchymal renal haematoma in the absence of antithrombotic therapy and trauma. SRH is most frequently caused by vascular malformations, vasculitides such as polyarteritis nodosa, or occult vascular renal tumours such as renal cell carcinoma or angiomyolipoma. Renal neoplasms are the most common cause of SRH, accounting for up to 65% of all cases[2,3].
Patients with SRH may present with insidious-onset flank pain, a palpable flank mass, and hypovolemic shock; these are known as ‘Lenk's triad’ and are associated with retroperitoneal haematoma[1].
The diagnosis can be complex, as SRH can mimic some acute abdominal pathologies such as aortic dissection. SRH is often incidentally discovered on ultrasound or contrast-enhanced CT scan. Ultrasound is valuable for its rapid identification of the condition, but its findings must be confirmed with a CT scan, which also gives information regarding the cause of the haemorrhage. If the CT scan is unclear regarding aetiology, an angiogram is recommended by many authors. If radiological investigations fail to identify the cause, surgical exploration and biopsy is recommended[1,2].
There are several management recommendations, which depend on the presence of active bleeding and the patient's general haemodynamic status. Initial surgical reports suggested emergency nephrectomy for all cases. However, recent studies suggest a trial of conservative therapy with hydration, pain management, blood product replacement, and volume resuscitation with intravenous fluids; if there is concern for an infectious aetiology, appropriate antibiotic therapy should be started. Selective arterial embolization is another method to control active bleeding, and many authors recommend it as the definitive therapy. However, nephrectomy is still the first-line approach. As such, therapeutic recommendations often reflect the experience of the author[3].