ABSTRACT
Introduction: Ischaemic anterior thalamic lesions are rare and can present with disturbances of behaviour and memory. We describe a patient with post-cardiac arrest thalamic stroke.
Case description: A 63-year-old man presented with cardiac arrest, was resuscitated after receiving life support, and showed no lesions on computed tomography. Three days later, he presented with short-term memory disturbance and disorientation, with a de novo anterior thalamic lesion.
Conclusion: The anterior thalamic nucleus, supplied by the posterior communicating artery, is part of the Papez circuit and has a role in modulating behaviour and memory. An anterior thalamic syndrome presents with no sensory-motor deficits.
LEARNING POINTS
- Anterior thalamic stroke is a rare condition and can present with disturbances of short-term memory and behaviour; it usually does not include any motor or sensory deficits.
- Thalamic stroke can occur due to global hypoxia, such as during cardiopulmonary arrest.
KEYWORDS
Anterior thalamic stroke, post-cardiopulmonary arrest stroke, limbic thalamus
INTRODUCTION
The human thalamus is the largest structure in the diencephalon and is located laterally to the third ventricle and beneath the superior portion of the lateral ventricle. Its anterior pole forms the posterior border of the interventricular foramen. The geniculate bodies are located in its postero-ventral extremity. A Y-shaped thin lamina of white matter separates the thalamic grey matter into three main segments: the anterior, medial and lateral. Each nucleus has its own afferent and efferent fibres connecting with the rest of the central nervous system, such as the cerebral cortex, brainstem nuclei, basal ganglia and hippocampus.
The main blood supply for the thalamus derives from branches of the posterior communicating and cerebral posterior arteries, and can be divided into four main arterial segments: the anterior, paramedian, infero-lateral and posterior. The anterior segment is mainly supplied by branches of the posterior communicating artery, while the remaining three segments are supplied by perforating branches of the first two segments of the posterior cerebral artery[1–3].
The anterior segment presents the anterior thalamic nucleus, closely related to the limbic system, which includes the hippocampus. Through fibre tracts of the anterior cingulum, the anterior thalamus has close connections with the subicular and retrosplenial cortex, as well as the orbitomedial prefrontal cortex. Consequently, the anterior thalamus has an important role in the regulation of episodic memory, cognition and executive functions. Lesions of the anterior thalamus or its mamillo-thalamic connections are responsible for the disturbance of episodic memory usually seen in thalamic infarcts and in Wernicke-Korsakoff syndrome[2].
We present the case of a patient with memory and behaviour disturbance after an anterior thalamic ischaemic stroke.
CASE DESCRIPTION
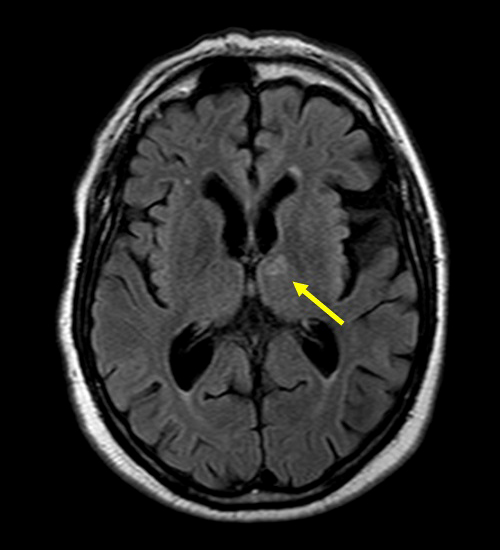
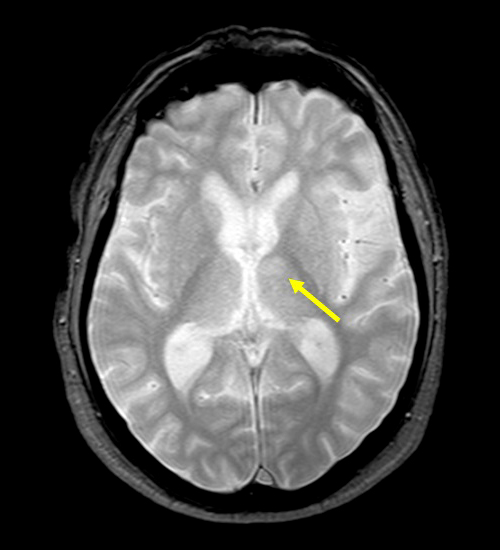
We describe a 63-year-old man with a history of long-standing bipolar disorder. He was admitted in our Emergency Room (ER) after a witnessed outpatient cardiac arrest, with return of spontaneous circulation after 5 minutes of basic life support, and a Glasgow Coma Scale score of 15 after resuscitation. Aetiology remained unclear; a head computed tomography scan (CT scan) showed no structural or ischaemic abnormalities, and the patient was rapidly discharged. However, 3 days later, he was disoriented, with periods of mental agitation and short-term memory disturbance, as well as dysarthria. A second CT scan, complemented with magnetic resonance imaging, revealed an ischaemic lesion in his left anterior thalamus, with no evidence of small vessel disease (Figs 1 and 2). He was again admitted to our internal medicine ward for stroke aetiology study and follow-up. There was complete resolution of symptoms in 3 days. The Holter monitor showed no malignant dysrhythmia, the carotid arterial Doppler was innocent, and a transthoracic echocardiogram showed no structural abnormalities. After consultation with Neurology, this anterior thalamic stroke was considered to be a result of post-cardiac arrest cerebral insult. The patient is medicated with aspirin and statin.
Figure 1. Flair MRI sequence showing a hyperintense lesion in the left anterior thalamic nucleus
Figure 2. T2W MRI sequence showing a hyperintense lesion in the left anterior thalamic nucleus
DISCUSSION
The thalamic functional blood supply is complex and includes four main territories: the anterior or tuberothalamic, paramedian or medial, inferolateral and posterior. The anterior portion is supplied by tuberothalamic branches of the posterior communicating artery. The paramedian group is supplied by thalamic perforating branches of the first segment of the posterior cerebral artery. The inferolateral segment is supplied by the thalamogeniculate branches coming from the second segment of the posterior cerebral artery. The posterior group is supplied by branches of the posterior choroidal arteries, branches of the posterior cerebral artery[1,3].
During an episode of cardiac arrest, global hypoxia ensues and is responsible for cerebral ischaemic insult, which can present after resuscitation. The most frequently injured structures include the hippocampus, cerebellum, basal ganglia, frontoparietal cortex and thalamus. A hypoxic ischaemic thalamic lesion can present with a myriad of symptoms, depending on the affected segments and fibre tracts, with secondary insult to cortical plasticity due to inadequate thalamic input. A thalamic lesion can have a prognostic impact after resuscitation, since most sensory and corticosubcortical data are modulated by this structure, including memory and awareness. There are few related cases of post-resuscitation thalamic ischaemic stroke, and the majority include the posteromedial segment[1,4].
The anterior thalamic nucleus is located on the rostral part of the dorsal thalamus and has three secondary nuclei: the anteromedial, anterodorsal and anteroventral. This anterior nuclei group is part of the limbic circuit of Papez, in close proximity to the hypothalamic mamillary bodies to which it is connected through the mamillo-thalamic tract of Vicq-d’Azyr. By receiving afferents from the hippocampus, the anterior thalamus has an important role in modulating short-term memory, as well as awareness and cognition. As such, an ischaemic lesion of the anterior thalamus can present with disturbances of these components; it usually causes no motor or sensory abnormalities[3].
Our patient experienced a post-resuscitation anterior thalamic stroke with memory, awareness and behavioural disturbances. Clinicians should be aware of this rare presentation of a common condition.