ABSTRACT
Acute myocarditis is a well-recognized condition attributable to a variety of viral illnesses. Common viral aetiologies include enteroviruses including coxsackie, adenovirus, influenza, echovirus, parvovirus B19 and herpesvirus. A high index of suspicion, early diagnosis, and prompt management with supportive anti-failure measures, and in selected cases immunosuppressive therapies including high-dose steroids, might be considered for better outcomes. The authors report a case of sudden onset of acute heart failure complicated by cardiogenic shock caused by viral myocarditis in a patient who initially presented with norovirus gastroenteritis. She had no previous cardiac history or significant cardiovascular risk factors. Prompt medical management for cardiogenic shock for norovirus-induced myocarditis was started, her symptoms gradually improved, and she was discharged safely on regular follow-up.
LEARNING POINTS
- Viral myocarditis exhibits a wide spectrum of symptoms ranging from non-specific prodromes such as fatigue and myalgia to chest pain, life-threatening arrhythmias, fulminant heart failure, or even sudden cardiac death.
- Common viral aetiologies for myocarditis include enteroviruses including coxsackie, adenovirus, influenza, echovirus, parvovirus B19 and herpesvirus.
- A high index of suspicion, early diagnosis, and prompt management with supportive anti-failure measures, and in selected cases immunosuppressive therapies including high-dose steroids, might be considered for better outcomes in cases of acute myocarditis.
KEYWORDS
Myocarditis, gastroenteritis, enteric viruses, norovirus
INTRODUCTION
Acute myocarditis is a well-recognized condition attributable to a variety of viral illnesses. Common viral aetiologies include enteroviruses including coxsackie, adenovirus, influenza, echovirus, parvovirus B19 and herpesvirus. The authors report a case of sudden onset of acute heart failure caused by viral myocarditis in the setting of norovirus gastroenteritis.
CASE DESCRIPTION
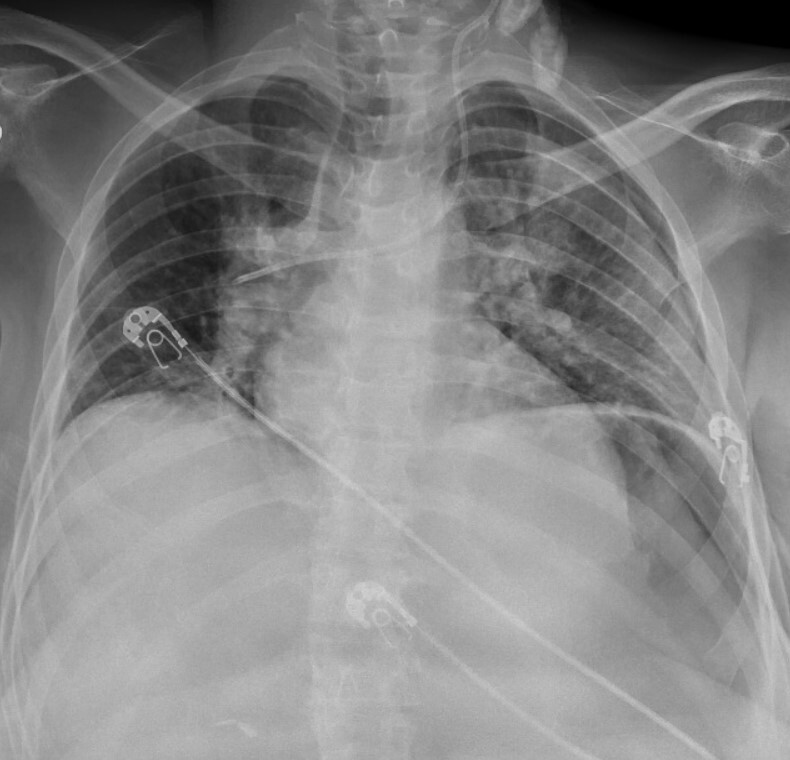
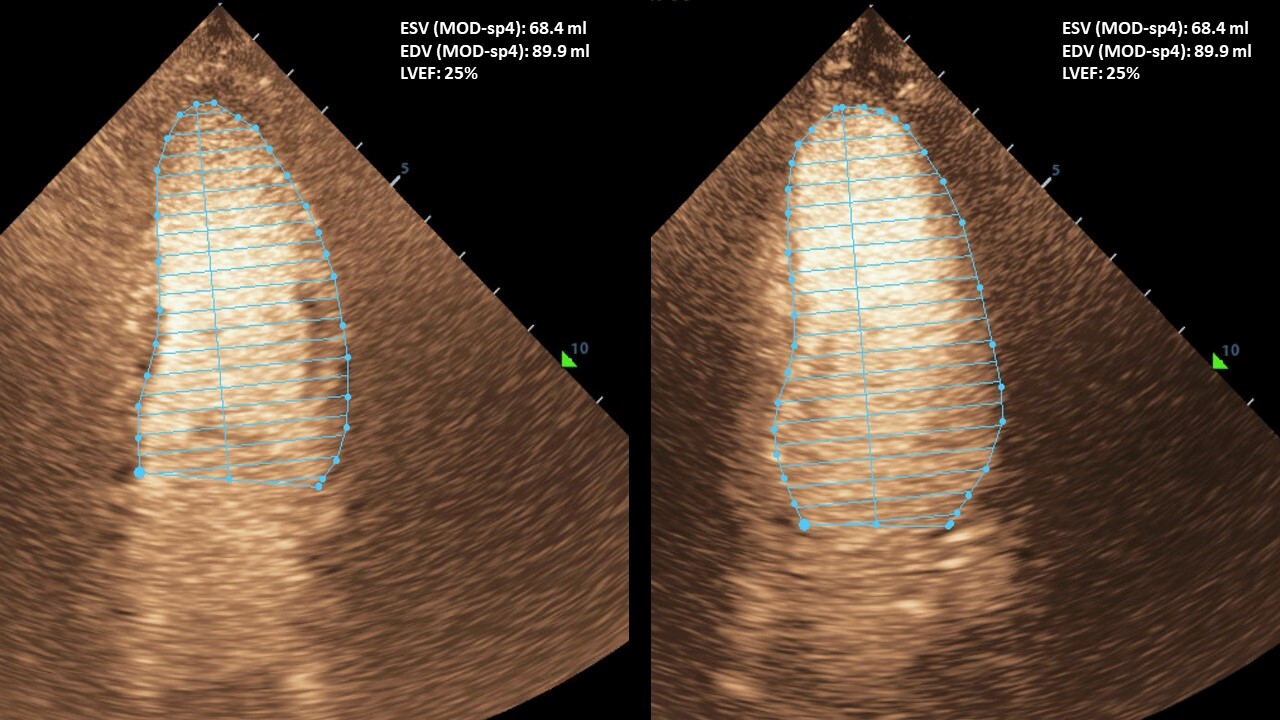
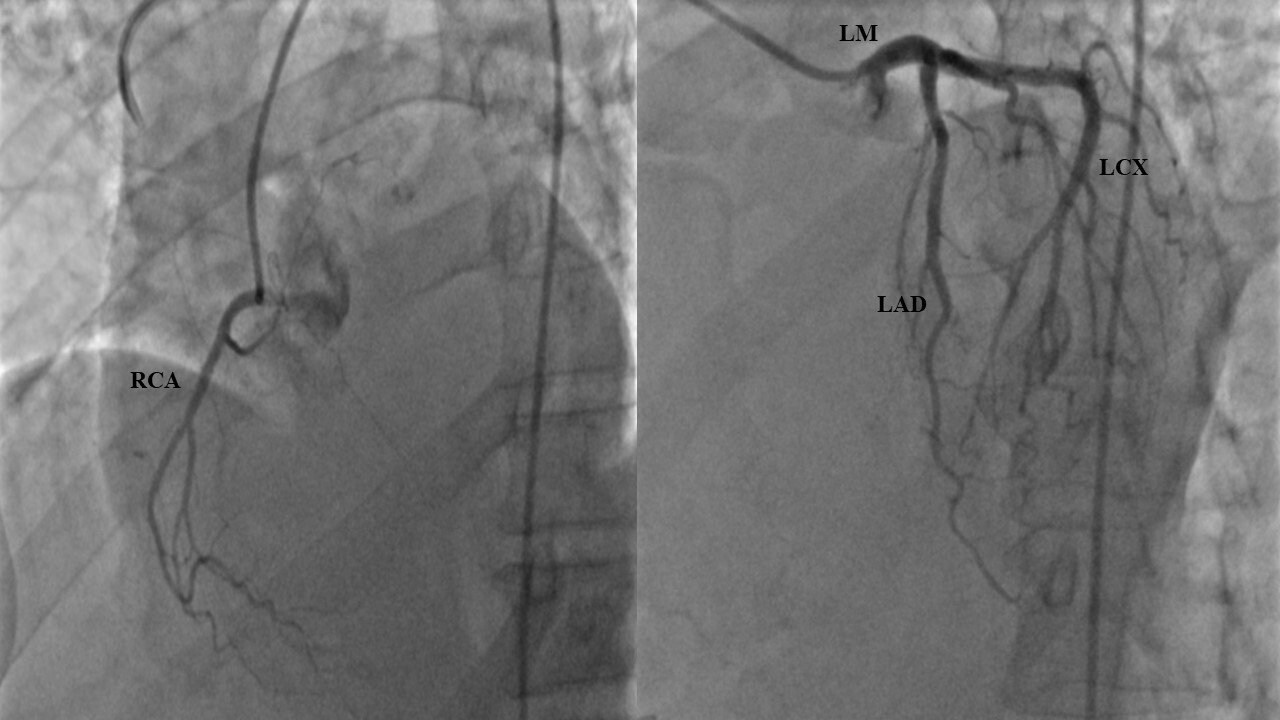
A 46-year-old woman with a past medical history of cerebral palsy, epilepsy and profound intellectual disability, initially presented complaining of a 1-day history of irritability, worsening nausea, vomiting, inability to tolerate oral intake, and recurrent episodes of watery diarrhoea. Initially, no cardiopulmonary symptoms, including chest pain or dyspnoea, were reported. On initial clinical examination, the patient was distressed, afebrile with a temperature of 36.7°C, hypotensive with a blood pressure of 85/55 mmHg, tachycardic with a heart rate of 110 beats per minute, and tachypnoeic with a respiratory rate of 20 per minute and oxygen saturation of 92% on room air. Marked abdominal pain with guarding, jugular venous dilatation, and bilateral basal crepitations were noted. Initial laboratory work-up revealed elevated renal and liver functions, lactic acidosis, and markedly elevated troponin and pro-B-type natriuretic peptide (BNP). Chest x-ray showed cardiomegaly and pulmonary congestion (Fig. 1). Electrocardiogram (ECG) showed sinus tachycardia with a heart rate of 110 beats per minute otherwise unremarkable. Urgent transthoracic echocardiography (TTE) showed new-onset global hypokinesia of all myocardial segments with an estimated left ventricular systolic function (LVEF) of 25% (Fig. 2). The initial differential diagnosis was myocarditis versus acute coronary syndromes. Based on TTE results and troponin elevation, emergent coronary angiography was performed showing non-obstructive coronary artery disease (CAD) (Fig. 3).
The patient had two negative sets of blood cultures and a negative polymerase chain reaction (PCR) respiratory viral panel that included adenovirus, influenza, parainfluenza species, SARS-CoV-2, human metapneumovirus, rhinovirus/enteroviruses, and respiratory syncytial viruses. A PCR viral enteric panel that included Clostridium difficile strains, Yersinia enterocolitica, rotavirus, Shigella, Salmonella, Campylobacter, Vibrio species, and norovirus tested positive for norovirus. Per her family’s request, no further invasive diagnostic procedures such as endomyocardial biopsy (EMB) for further assessment of possible myocarditis as a probable cause of acute heart failure and cardiogenic shock, were pursued. The patient was promptly started on diuretics, vasopressors and dobutamine infusion with significant improvement in her haemodynamic instability and gradual weaning of pressor and inotropic support. She was discharged safely on regular outpatient follow-ups.
Figure 2. Contrast transthoracic echocardiography showing reduced left ventricular systolic function with an estimated left ventricular ejection fraction of 25%
DISCUSSION
Viral myocarditis exhibits a wide spectrum of symptoms ranging from non-specific prodromes such as fatigue and myalgia to chest pain, life-threatening arrhythmias, fulminant heart failure, or even sudden cardiac death. Common viral aetiologies include enteroviruses including coxsackie, adenovirus, influenza, echovirus, parvovirus B19 and herpesvirus[1]. Norovirus is a common cause of viral gastroenteritis, typically with a mild and short disease course primarily affecting children younger than 5 years of age. Common symptoms include nausea, vomiting, abdominal pain and cramping, watery diarrhoea, myalgias, headache and chills. Some patients report a predominance of diarrhoea, while others report nausea and vomiting as primary symptoms that usually last 2–3 days with complete resolution[2]. Previously reported sequelae associated with norovirus range from mechanical complications (Boerhaave’s syndrome, intussusception) and acute and chronic inflammatory effects (necrotizing enterocolitis, pneumatosis intestinalis, intestinal perforation), to extraintestinal manifestations (renal and liver failure, convulsions, encephalopathy, Guillain-Barré syndrome and heart failure)[3].
The exact pathophysiology of norovirus-induced myocarditis remains unknown. Possible explanations include direct cardiomyocyte invasion, secondary immune activation-mediated damage, and endothelial damage[4]. Another proposed mechanism is based on binding between the viral P2 domain and human histo-blood group antigens (HBGAs) namely A/B, H and Lewis, resulting in the stimulation of CD4+ cells with subsequent production of IFN-γ and IL-2 resulting in myocarditis[5,6]. Initial laboratory work-up for possible myocarditis includes elevated troponin and BNP levels. ECG is usually abnormal in myocarditis. Although ECG signs are neither specific nor sensitive, myocarditis should be considered based on the following ECG changes: new PR interval prolongation, atrioventricular block, ventricular arrhythmias, frequent premature ventricular complexes, ST depression, or diffuse T-wave inversions[7]. Echocardiographic signs suggestive of myocarditis include LVEF changes, diastolic function, new wall motion abnormalities, or pericardial effusion. Echocardiography can also be used to monitor treatment response. Cardiac magnetic resonance imaging (CMR) is a validated non-invasive modality to diagnose myocarditis. Diagnostic criteria include signs of myocardial oedema such as abnormal findings on T2 mapping or T2-weighted images or signs of non-ischaemic myocardial injury such as abnormal findings on T1 mapping, late gadolinium enhancement (LGE), or extracellular volume fraction, while supportive criteria include signs of pericarditis such as pericardial effusion or abnormal LGE/T2 or T1 findings in the pericardium, or left ventricular systolic dysfunction such as regional or global wall motion abnormalities[7]. Endomyocardial biopsy (EMB) is the gold standard method for diagnosis. Histological criteria require inflammatory infiltrate (global or focal with patchy disease) and myocardial necrosis. Although coronary angiography does not rule out myocarditis, it is often done to exclude CAD as a cause of similar clinical presentations, elevated biomarkers, ECG changes, or imaging abnormalities[7].
This case report showed a temporal relationship between the onset of gastroenteritis and the abrupt onset of acute heart failure symptoms in a patient with no previous cardiac history or significant cardiovascular risk factors. Her clinical presentation was consistent with acute myocarditis, which should be considered in patients without typical cardiovascular risk factors presenting as more common conditions such as acute coronary syndromes (ACS) or de novo acute heart failure, and in patients with electrical instability, or rapidly evolving conduction abnormalities such as widening of the QRS complex or PR prolongation. Based on the timeline of her clinical, laboratory and echocardiographic signs of acute heart failure and after CAD exclusion by coronary angiography, a diagnosis of norovirus-induced myocarditis complicated by acute heart failure was pursued. Ideally, CMR or endomyocardial biopsy would be the next step to confirm the diagnosis. However, given her comorbidities and her family’s request, neither was done and she was started on supportive management and corticosteroids with gradual improvement of her symptoms.
Patients with acute myocarditis should receive guideline-directed medical treatment for heart failure and arrhythmias. In addition, physical activity should be restricted during the acute phase of myocarditis and for at least 6 months in athletes and non-athletes. Immunosuppressive therapies might be considered after active infection is ruled out on EMB by PCR. Previous reports indicate that corticosteroids do not reduce mortality but may improve cardiac function. Corticosteroids might be considered in cases with severe ventricular dysfunction and/or life-threatening arrhythmias. There are no data regarding the efficacy of antiviral therapies. Preliminary data on interferon-beta treatment suggest that it can eliminate cardiotropic viruses and improve left ventricular function and NYHA functional class[7]. Data regarding the interaction between viral infections suggested that respiratory viruses can concurrently or sequentially infect the respiratory tract and result in virus-virus interactions. Infection by a first virus could enhance or reduce infection by and replication of a second virus, resulting in positive (additive or synergistic) or negative (antagonistic) interaction[8]. Limited data regarding enteric viruses and their interaction with enteric bacteria might affect the outcomes of infection[9]. Further research is required to further determine the outcomes of virus-virus interactions and virus-bacteria interactions.
CONCLUSIONS
Acute myocarditis is a well-recognized condition attributable to a variety of viral illnesses. A high index of suspicion, early diagnosis, and prompt management with supportive anti-failure measures, and in selected cases immunosuppressive therapies including high-dose steroids, might be considered for better outcomes in cases of acute myocarditis.