ABSTRACT
A brain abscess is an enclosed focal infection within the brain that is either initiated by haematogenous seeding or spreads contiguously from oto-sinusitis, local trauma or neurosurgery. We describe the case of a 71-year-old man presenting with acute confusion and unilateral neurology in the absence of systemic signs of sepsis or associated laboratory biomarkers. While his initial clinical presentation mimicked an acute cerebrovascular event or brain tumour, he was subsequently diagnosed with a particularly large spherical temporal lobe brain abscess of 5 cm diameter on neuroimaging. This abscess was treated successfully with craniotomy, evacuation and a prolonged course of anti-microbials, enabling him to return to his pre-morbid level of functioning. His prolonged course of anti-microbials was complicated by candidaemia and colonisation of an indwelling central venous catheter that was treated successfully with anti-fungals.
LEARNING POINTS
- A high index of suspicion for brain abscess should be maintained when a ring-enhancing lesion is found on neuroimaging, even in the absence of signs of sepsis or associated laboratory biomarkers.
- Commensal yeasts may colonise indwelling lines in patients treated with long-term broad-spectrum antibiotics.
- Distracting concomitant diagnoses may delay recognition of the primary pathological process.
KEYWORDS
Otogenic brain abscess, candidaemia
CASE DESCRIPTION
We describe the case of a 71-year-old man who was brought in by ambulance to our emergency department with a 24-hour history of confusion, headache, new onset left arm and left leg weakness, ataxia, left facial droop and dysphasia on a background of a recent COVID-19 diagnosis made on a lateral flow test.
Three days before his presentation, he and a family member experienced subjective fevers, rigors and flu-like symptoms which prompted lateral flow tests which were returned as positive for COVID-19. These fevers had settled approximately 36 hours prior to his presentation without any antibiotic use in the community. His neurological symptomatology was of acute onset with rapid development of confusion, obtundation, headache, ataxia, dysphasia, left facial weakness, and left upper and lower limb weakness over approximately 24 hours.
He had a medical history positive for dyslipidaemia, hypertension, glaucoma, asthma and polymyalgia rheumatica. He had undergone mastoid surgery for mastoiditis approximately 10 years previously, and a collateral history revealed he had leaked fluid from his ear since. Prior to his deterioration, he had been independent in all activities of daily living.
He had no known drug allergies. He was prescribed esomeprazole 20 mg daily, olmesartan/amlodipine 40 mg/10 mg daily, aspirin 75 mg daily, salmeterol/fluticasone 25/250 µg twice daily, and one drop of travoprost in each eye daily. He did not smoke tobacco or drink alcohol.
On examination, his heart rate was 63 beats per minute, blood pressure was 131/78 mmHg, temperature was 36.1°C (and remained normothermic throughout the initial weeks of his presentation), respiratory rate was 16 breaths per minute and oxygen saturations were 100% on room air. His cardiovascular, respiratory and abdominal examinations were unremarkable. His neurological examination was negative for signs of meningism, in that both Kernig’s and Brudzinski’s signs were negative, he had no vomiting and he complained of no specific photophobia. However, examination was remarkable for facial droop and decreased power (3/5 on the Medical Research Council Scale for Muscle Strength) on the left side. He additionally displayed overt signs of dysphasia, emotional lability and confusion.
METHODS AND PROCEDURES
Investigations
His chest x-ray was unremarkable. His electrocardiogram showed an incomplete right bundle branch block and normal sinus rhythm at 65 beats per minute.
His COVID-19 PCR test was returned as positive. Renal function tests, liver function tests, bone profile, a blood glucose, troponin I and coagulation profile were within normal ranges. His CRP was 5 and his full blood count was remarkable only for mild neutrophilia of 7.16×109 cells per litre, just above the upper limit of normal of 7×109.
An urgent CT brain with contrast was reported as showing a large cystic structure in the right temporal lobe with marked surrounding oedema with peripheral enhancement consistent with a primary cystic neoplasm, cystic metastatic disease, lymphoma or an abscess.
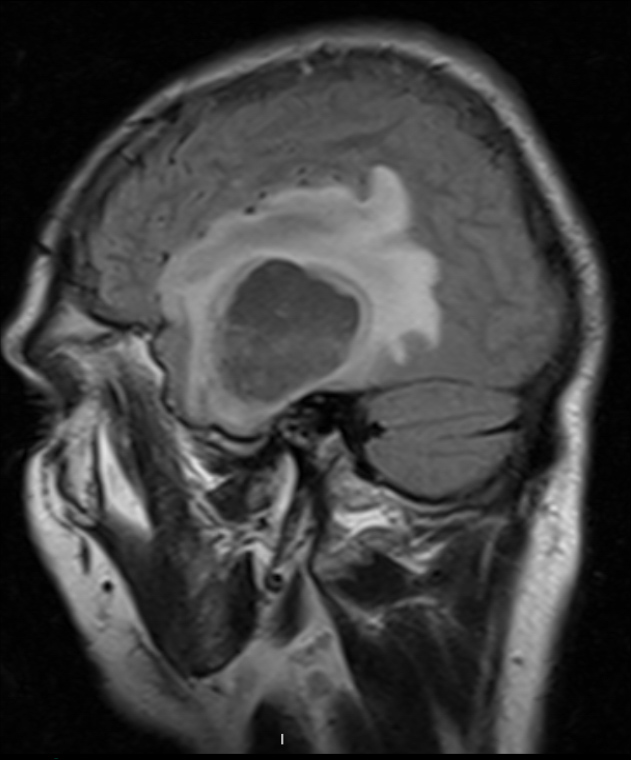
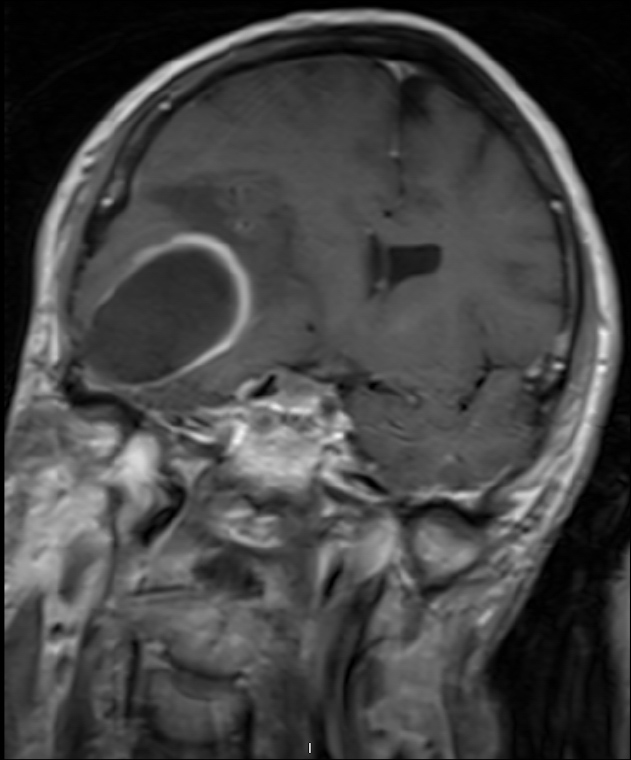
This prompted an MRI of the brain (Figs. 1 and 2) with contrast which was reported as showing an unusually large spherical intracranial abscess lying directly above an expanded middle ear cavity, a cholesteatoma and focal erosion of the tegmen tympani. Its diameter was 5 cm.
Figure 1. T2 weighted sagittal MRI Brain showing a large spherical intracranial abscess
Figure 2. T1 weighted coronal MRI Brain showing a large spherical intracranial abscess and focal erosion of the tegmen tympani
Intervention
The patient was transferred emergently to a tertiary centre for craniotomy and neurosurgical evacuation of this right temporal lobe abscess. Abscess fluid culture yielded Dermabacter hominis.
He was commenced on intravenous vancomycin, ceftazidime and metronidazole, which were continued for 9 weeks. He received levetiracetam for seizure prophylaxis.
HIV serology and serum protein electrophoresis were returned as negative.
As he neared completion of his course of intravenous antibiotics, he became pyrexial (for the first time since his initial presentation) and grew a Candida parapsilosis on blood cultures. His peripherally inserted central catheter was removed and the tip grew an identical organism. An echocardiogram did not show any signs of endocarditis. Fundoscopy did not yield any evidence of fungal endophthalmitis. He was treated with a 1-week course of intravenous anidulafungin that was subsequently switched to oral fluconazole for 2 weeks.
Resolution
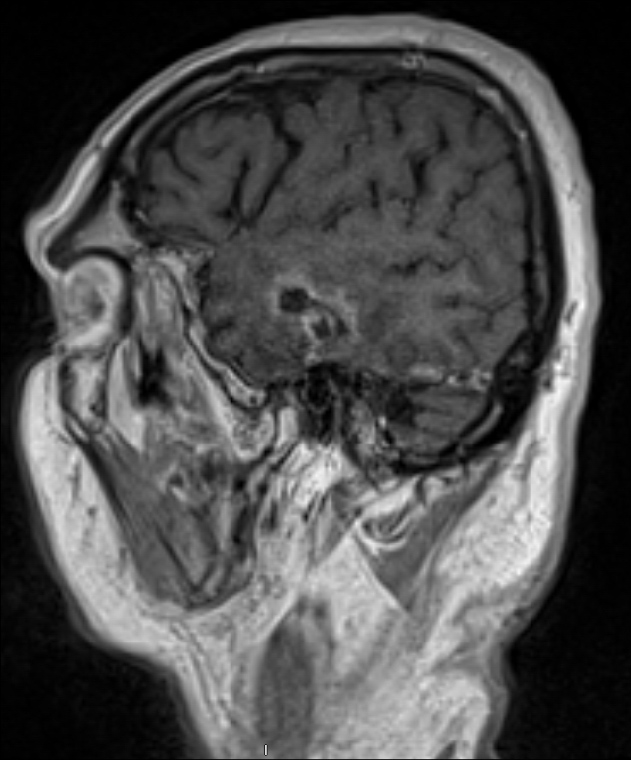
Subsequent imaging over 11 weeks showed resolution of the abscess (Fig. 3) and the patient made an excellent clinical recovery with a return to his pre-morbid functioning and a return to driving his car on the road.
DISCUSSION
A brain abscess is an enclosed focal infection within the brain that is either initiated by haematogenous seeding or spreads contiguously from oto-sinusitis, local trauma or neurosurgery. Some 50–60% of brain abscesses are otogenic in origin, and approximately 55% thereof are located in the temporal lobe[1,2]. Brain abscesses are often complicated by meningitis and they have an approximately 20% mortality risk[3,4].
Treatment of a brain abscess is typically surgical, with drainage or excision achieved either via a burr hole, mastoidectomy or craniotomy. This is then followed by an extended course of anti-microbial therapy[5].
A cerebrovascular accident (CVA), brain tumour and brain abscess can be distinguished from each other by key differences in the history. CVAs are of rapid onset, in the order of seconds to minutes, and are not usually associated with pyrexia or elevation of inflammatory markers. Brain tumours also are not accompanied by signs of infection and typically provoke neurological symptomatology over weeks to months, although they can also provoke more acute events such as seizures and other focal neurology. Brain abscesses are typically subacute, evolving over days to weeks. They are associated with headache in 69% of cases, with neurological deficits in 48% of cases, and with clinical (fever in 48%) and biochemical signs of infection (60% of cases[6]). This triad of headache, fever and neurological deficit was noted in one review as being complete in only one fifth of patients diagnosed with brain abscess[7]. Another systematic review found a mean duration of symptoms prior to diagnosis of brain abscess of 8.3 days[6].
This patient manifested headache and focal neurological deficit; however, his presentation was unusual given that his deficits evolved over a very short time frame (24 hours being much less than the mean of 8 days mentioned in the literature) and were associated with both an absence of pyrexia at presentation and with an absence of a marked rise in his CRP or neutrophils. Accordingly, initial impressions were one of acute stroke at presentation to the emergency department. These then gave way to a putative diagnosis of brain tumour after neuro-imaging before a final diagnosis of brain abscess was made. His abscess, given his history of otorrhoea and the MRI findings of a focal defect in the tegmen tympani, was likely otogenic in origin. His presentation was also confounded by the distracting diagnosis of COVID-19 made some 3 days prior to his presentation, which may have obfuscated delineation of the timeline of his symptomatology.
Accordingly, this case highlights the importance of entertaining a high index of suspicion for brain abscess in those presenting with a peripherally enhancing brain lesion and acute neurology even in the absence of markedly deranged inflammatory markers or signs of sepsis. It also emphasises the importance of being aware that concomitant diagnoses may distract from the primary causative pathology. It also underscores the risk of selection of commensal yeasts and their colonisation of indwelling lines in patients treated with long-term broad-spectrum antibiotics[8].