ABSTRACT
Introduction: Groove pancreatitis is a rare form of chronic pancreatitis. Its radiological diagnosis is challenging and it can be difficult to distinguish from pancreaticoduodenal malignancy.
Case description: A 64-year-old woman was admitted to our internal medicine ward after she contracted severe COVID-19 pneumonia requiring mechanical ventilation. She presented with right upper abdominal pain, and a CT scan showed pancreaticoduodenal inflammatory tissue; malignancy was ruled out.
Conclusion: Diagnosing groove pancreatitis is challenging and malignancy must be quickly excluded. No cases of COVID-19-associated groove pancreatitis have been previously described.
LEARNING POINTS
- Groove or paraduodenal pancreatitis is a rare form of chronic pancreatitis, and usually associated with alcohol use.
- The differential diagnosis includes pancreaticobiliary and duodenal malignancies.
- Radiological diagnosis is challenging and treatment is usually supportive.
KEYWORDS
Groove pancreatitis, COVID-19-related gastrointestinal disease
INTRODUCTION
Groove pancreatitis (GP), also known as paraduodenal pancreatitis, is a rare and under-recognized form of focal chronic pancreatitis. It affects the groove located between the pancreatic head, the adjacent duodenum and the terminal common bile duct. It can be divided into two forms. The pure form affects only the pancreaticoduodenal groove, while the segmental form is centred in the groove and extends medially into the pancreatic head. A definitive diagnosis can be difficult due to inability to distinguish it from a pancreatic, duodenal or ampullary malignancy[1].
Its symptoms are the same as in other types of chronic pancreatitis, with recurrent upper abdominal pain, nausea, and weight loss from malnourishment. Jaundice, however, is uncommon, despite the involvement of the common bile duct. These features often suggest an underlying malignancy, making it even more difficult to diagnose. The average duration of symptoms is usually 3–6 months. Most patients are male and aged 40–60 years, with a history of chronic alcoholism and, in a lower percentage, smoking[1].
Its pathogenesis remains controversial, although a number of different theories have been proposed. Histopathological features include granulation tissue, functional obstruction of the minor papilla or duct of Santorini, with secondary dilated pancreatic ducts; hyperplasia of Brunner glands resulting in stasis of pancreatic secretions in the dorsal pancreas; and involvement of the pancreaticoduodenal groove by fibrotic inflammatory alterations[2,3].
Biochemical markers are of limited use, as both pancreatic enzymes and tumour markers such as CEA and CA-19.9 are within normal ranges. If the common bile duct is obstructed, bilirubin levels can be elevated. Alkaline phosphatase levels can be raised even in the absence of ductal obstruction[1].
The differential diagnosis includes pancreatic adenocarcinoma of the head of the pancreas, duodenal adenocarcinoma, acute pancreatitis, ampullary carcinoma, and duodenal gastrointestinal stromal tumour[1–3].
The radiological findings of GP vary between the pure and segmental forms. On CT scans, in the pure form, there is often soft tissue in the groove, with ill-defined inflammatory changes, with delayed enhancement in the late phase of dynamic CT; there may be thickening of the medial duodenal wall. In the segmental form, the enlargement of the pancreatic head is the dominant finding, and involvement of the groove is often obscured. Regardless of the form of GP, there is usually no diffuse retroperitoneal inflammatory change, which is usually observed in acute oedematous pancreatitis. Pancreatic ductal irregularities are common in GP cases, especially in its segmental form. Findings on MRI largely mirror those seen on CT. Magnetic resonance cholangiopancreatography (MRCP) is an important diagnostic tool in several pancreaticobiliary diseases, and it can reveal abnormalities of the distal common bile duct and distal pancreatic duct, both narrowed near the ampulla[2,3].
Treatment is usually supportive, similar to cases of acute oedematous and chronic pancreatitis. It typically consists of a combination of fasting, parenteral nutrition and cessation of smoking or alcohol use. In the chronic setting, some patients may present with severe pancreatic insufficiency and may require definitive surgery, such as a Whipple procedure (pylorus-sparing pancreaticoduodenectomy). Endoscopic drainage of the minor papilla has been shown to be effective[1].
SARS-CoV-2 infection has a wide spectrum of clinical features, mostly affecting the respiratory system. Acute pancreatitis is a common gastrointestinal disease with many causes, most frequently requiring hospitalization. Its aetiology remains unknown in almost 25% of cases, but viral pancreatitis has been well-described in the literature.
COVID-19-related acute pancreatitis seems to lead to more severe disease and mortality. We present a case of viral GP.
CASE DESCRIPTION
We present the case of a 64-year-old woman with a medical history of human immunodeficiency virus (HIV-2) infection with excellent control under abacavir, dolutegravir and lamivudine. She was initially admitted in January 2021 to our Intensive Care Unit for hypoxaemic respiratory failure due to severe COVID-19 pneumonia, requiring mechanical ventilation. A contrast-enhanced CT scan showed a subsegmental pulmonary embolism in the right inferior lobar artery, with no right cardiac chamber failure, and she was started on enoxaparin. The patient was successfully weaned off the ventilator and extubated, and afterwards transferred to our internal medicine ward.
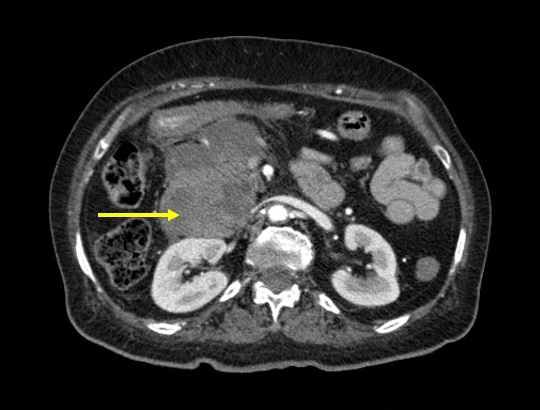
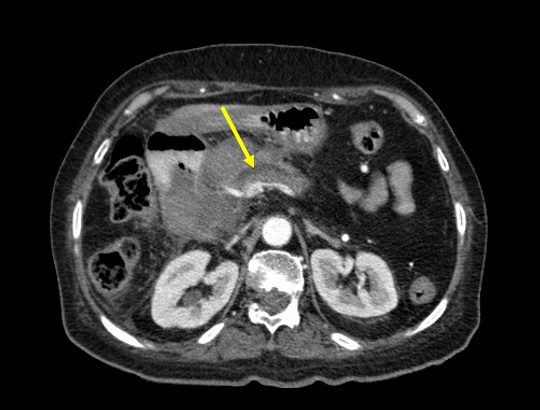
On the 39th day after admission, she presented with upper right abdominal pain; she had elevated bilirubin, alkaline phosphatase and gamma-glutamyltransferase levels, with normal amylase, CEA and CA-19.9 levels. A contrast-enhanced CT scan showed inflammatory tissue adjacent to the pancreatic head and in the pancreaticoduodenal groove, with narrowing of the distal bile duct (Figs. 1 and 2). Supportive treatment consisted of fasting, parenteral nutrition and fluid resuscitation; enoxaparin therapy was stopped. MRCP, upper GI endoscopy and follow-up CT scans ruled out malignancy, with all biopsies documenting chronic inflammatory tissue. Multidisciplinary discussion with Gastroenterology and Radiology concluded a diagnosis of GP, triggered by her post-critical condition and severe COVID-19 disease. The patient maintains regular follow-up with Internal Medicine and Gastroenterology appointments.
Figure 1. A contrast-enhanced abdominal CT scan shows a large paraduodenal lesion (yellow arrow) in the pancreatic head in close proximity to the duodenal wall.
Figure 2. Abdominal CT scan (axial view) showing upstream dilation of the main pancreatic duct.
CONCLUSION
GP is a rare form of chronic pancreatitis centred into the pancreaticoduodenal groove. Most patients have a history of smoking and alcohol use. Its diagnosis can be challenging, as differentiating GP on the basis of clinical presentation, biological markers and imaging characteristics is very difficult. Knowledge of GP's radiological features may help the radiologist make the correct diagnosis.
COVID-19 infection mainly affects the lungs, but gastrointestinal manifestations have been linked to both mild and severe cases of COVID-19. Pancreatic injury in SARS-CoV-2 infection has several proposed mechanisms: it is thought to be mediated by angiotensin-converting enzyme 2 receptor expression in exocrine glands and islet cells of Langerhans. However, for a final diagnosis of viral pancreatitis, other likely causes must be excluded, such as alcohol consumption, gallstones and hypertriglyceridaemia. Although pancreatic injury is frequently documented, actual pancreatitis is uncommon. Most cases are considered idiopathic and more robust studies are needed to determine the relationship between pancreatitis and COVID-19. A Medline search using the following terms 'groove pancreatitis', 'COVID-19', 'acute pancreatitis' and 'COVID-19 pancreatitis', failed to identify any other cases of COVID-19-related GP in the literature[4]. Further studies are needed to establish the prevalence and significance of pancreatic disease in COVID-19 patients[1–3].