ABSTRACT
Introduction: The Fontan procedure is used to treat congenital heart defects and has improved long-term survival. Long-term complications include liver disease due to congestive hepatopathy. Fontan-related cirrhosis can manifest with ascites, gastrointestinal bleeding and encephalopathy.
Case description: A 43-year-old man with history of Fontan surgery was admitted with COVID-19 pneumonia. There was rapid clinical and neurological deterioration, with coma and shock. CT imaging showed thrombosis of the Fontan conduit. The patient was successfully subjected to recanalization of the Fontan circulation, with progressive improvement of coma.
Discussion: Fontan-associated liver disease is a major complication following the Fontan procedure. Clinicians must be aware of this pathology during patient follow-up.
LEARNING POINTS
- The Fontan procedure has improved the long-term survival of patients with single ventricle pathology.
- Fontan-associated liver disease is a result of haemodynamic changes associated with Fontan circulation; complications include hepatic encephalopathy and coma.
- Patients with Fontan circulation should be evaluated over time in order prevent and treat systemic complications.
KEYWORDS
Fontan circulation, Fontan-associated liver disease, hepatic encephalopathy
INTRODUCTION
The Fontan–Kreutzer procedure is used to treat several complex congenital heart defects which present with single functional univentricular hearts. First performed in 1968 by Francis Fontan, it has gained acceptance and achieved excellent short-term outcomes, ensuring that the systemic venous return is redirected into the pulmonary artery. However, long-term haemodynamic changes are caused by the surgery with several complications following slow but progressive heart failure that can affect virtually all organs. Fontan-associated liver disease (FALD) includes a wide group of functional and structural alterations secondary to congestive hepatopathy, with several stages ranging from asymptomatic steatosis to cirrhosis and hepatocellular carcinoma. Hepatic encephalopathy, defined as brain dysfunction secondary to liver failure, is a poorly documented event in FALD[1,2].
CASE DESCRIPTION
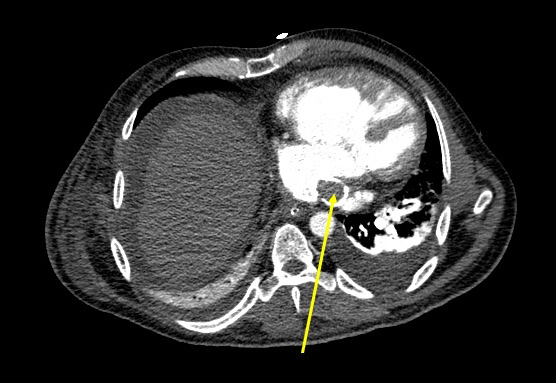
We present the case of a 43-year-old man, who underwent Fontan surgery at the age of 15 due to right isomerism with complete atrioventricular septal heart defect, which resulted in a total cavopulmonary connection. He was hospitalized in our internal medicine ward for moderate COVID-19, with acute respiratory failure due to bilateral pneumonia. On admission, he had mild thrombocytopenia (139,000/l), a prolonged INR of 1.64, and mild elevation of AST (133 U/l), ALT (153 U/l), GGT (176 U/l) and ALP (132 U/l), with total bilirubin and serum albumin within the normal range. There was no known history of previous liver disease, but liver ultrasonography revealed signs of chronic steatosis, with no focal lesions or biliary obstruction. Ten days after admission, there was rapid clinical and neurological deterioration, with the patient scoring 4 on the Glasgow Coma Scale (eye opening to pressure) with circulatory shock. Laboratory investigations revealed: thrombocytopenia (77,000/l), elevated D-dimer level (1.05 µg/ml), INR 1.50, slightly elevated AST and ALT (45 and 60 U/l, respectively), increased GGT (382 U/l), ALP (234 U/l) and an increase in total bilirubin (2.86 mg/dl), with a decrease in serum albumin (2.7 g/dl) and an increase in serum ammonia (217 µmol/l). Cranioencephalic CT scanning did not reveal any acute abnormalities. Thoracic and abdominal CT scanning revealed thrombosis of the Fontan conduit, with no signs of pulmonary embolism (Fig. 1). A diagnosis of COVID-19-related thrombosis was made, and the patient was started on vasopressors with norepinephrine and dobutamine, as well as mechanical ventilation.
Figure 1. A thoracic and abdominal contrast-enhanced CT scan shows thrombosis of the Fontan conduit (yellow arrow). There is also bilateral pleural effusion with subjacent atelectasis, and ascites
The patient was successfully submitted by cardiothoracic surgeons to recanalization of the Fontan circulation with four stents in tandem. He was started on heparin for 24 hours, then switched to warfarin. Additional therapy included rifaximin and lactulose. There was clinical recovery with progressive improvement in the hepatic encephalopathy and the level of consciousness, which improved from coma (GCS of 4) to a fully awake and conscious state (GCS 15).
CONCLUSION
Fontan surgery is one of the greatest advances in paediatric cardiology and is used to create an anastomosis between the systemic venous return from the vena cava and the pulmonary artery that results in the flow of systemic venous blood to the lungs without passing through a ventricle. This total cavopulmonary connection leads to chronic venous hypertension with hepatic congestion secondary to high-pressure non-pulsatile flow in the inferior vena cava[1–3].
Long-term systemic haemodynamic changes are associated with a considerable number of complications. Fontan failure may be precipitated by cardiac dysrhythmias, stenosis, and obstruction or thrombosis of the conduit. FALD is usually the first manifestation of Fontan failure, due to congestion and increased intrahepatic pressure with sinusoidal dilation. As such, most patients have mild hyperbilirubinaemia and an increase in GGT. As liver damage progresses, advanced fibrosis develops with portal hypertension, hypoalbuminaemia, prolonged coagulation times, and decreased platelet count. Possible complications of portal hypertension include ascites, gastrointestinal bleeding or hepatic encephalopathy[1,2].
Our patient had no known history of liver disease, but considering a Fontan surgery over 30 years ago, some degree of liver dysfunction would be expected. Initial laboratory findings at the current hospital admission were consistent with mild FALD. Thrombosis and resulting obstruction of the conduit was most likely due to a COVID-19-related prothrombotic condition, leading to further liver disease, with hepatic encephalopathy being the main manifestation. After stent implantation and conduit recanalization, there was clinical and laboratory improvement, supporting our diagnosis of FALD-related coma. It is a poorly documented event in FALD, and only three cases appear to have been published[2].
Establishing a causal relationship between the haemodynamic changes of the Fontan procedure and organ dysfunction can be challenging. Most patients with a Fontan conduit develop chronic liver disease and, as such, should be evaluated over time to determine their long-term risk of significant liver injury and the possible need for liver transplantation[1–3].