ABSTRACT
Primary thyroid lymphoma (PTL) is a rare malignancy of the thyroid gland which should be considered in patients with a rapidly growing cervical mass, especially in those with a history of Hashimoto’s thyroiditis. We present the case of a 53-year-old woman with a rapidly growing goitre with compressive symptoms. Computed tomography (CT) imaging was performed to examine the extent of disease and a biopsy showed B-cell non-Hodgkin lymphoma, stage I according to the Ann Arbor classification. The patient was immediately treated with high-dose prednisone for her compressive symptoms and after the diagnosis she received six cycles of R-CHOP (rituximab-cyclophosphamide-doxorubicin-vincristine-prednisone) chemotherapy. The patient has now been in remission for 12 months. We present this case to demonstrate the importance of awareness of PTL. Up to 10% of cases can be missed with fine needle aspiration cytology (FNAC), making it important to obtain a histological biopsy in rapidly growing goitres. In addition, establishing the correct diagnosis can in most cases prevent unnecessary surgical intervention. The preferred treatment with the best overall survival is chemotherapy with or without radiation therapy.
LEARNING POINTS
- Primary thyroid lymphoma is a rare malignancy of the thyroid gland which should be considered in rapidly growing goitres, especially when there is a history of Hashimoto’s thyroiditis.
- A histological biopsy is preferred to minimize misdiagnoses.
- Surgical intervention can typically be avoided with correct diagnosis and with the use of corticosteroids to reduce compression symptoms.
KEYWORDS
Primary thyroid lymphoma (PTL), thyroid malignancy, goitre
INTRODUCTION
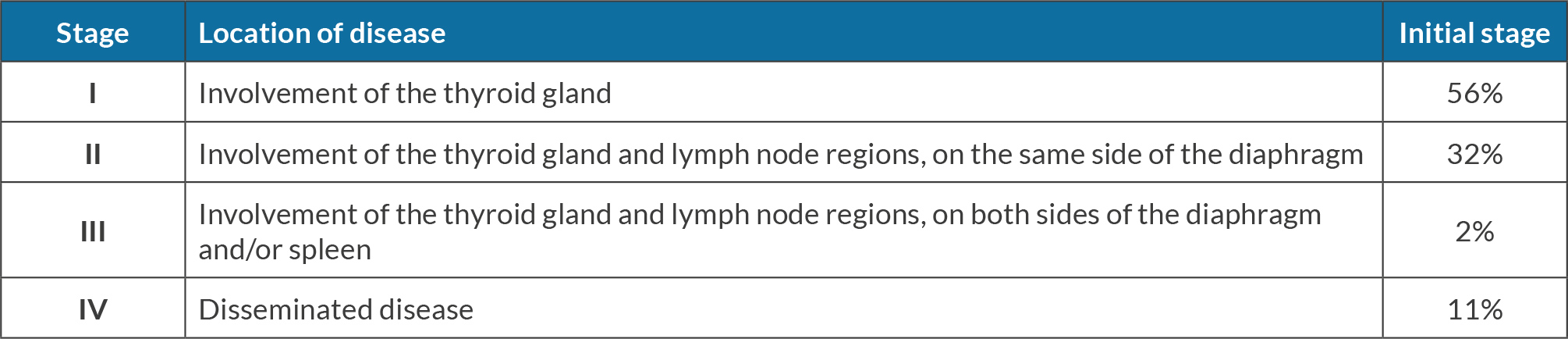
Primary thyroid lymphoma (PTL) is rare and accounts for up to 5% of all thyroid malignancies[1]. B-cell non-Hodgkin lymphoma is the most frequently encountered (50–80%) lymphoma in the thyroid gland[1]. Most patients present with a rapidly progressive cervical mass with signs of compression, such as inspiratory dyspnoea and/or stridor, dysphagia and hoarseness. B symptoms are relatively uncommon (10–20%)[1]. Despite its rarity, it is important for physicians to consider PTL, especially in patients with a history of Hashimoto’s thyroiditis as the prevalence in this group is 40–80 times higher than in the general population[1]. Transformation from thyroiditis to PTL occurs in about 0.5% of all patients[2]. Its pathogenesis consists of the development of lymphoid tissue, which is usually absent in the thyroid gland, probably due to chronic antigenic stimulation. PTL develops over approximately 9–10 years[3]. As in Hashimoto’s thyroiditis, women are mostly affected, with a median age of 59 years[4]. The cytological differentiation between thyroid lymphoma, lymphocytic thyroiditis and anaplastic carcinoma can be challenging. Therefore, fine needle aspiration cytology (FNAC) is less appropriate for diagnosing thyroid lymphoma and a core needle or open biopsy is often required to confirm the diagnosis[1]. In addition, treatment differs. For PTL, the general treatment is chemotherapy with or without radiation therapy, while for anaplastic carcinoma surgical resection is needed[1]. The Ann Arbor classification is used for staging[1] (Table 1) and survival is highly dependent on the stage, ranging from 80% for stage I to 36% for stage III and IV[3]. Moreover, the overall survival (OS) is lower for diffuse large B-cell lymphoma (DLBCL), with a mean 5-year OS for all stages of 44%, than for other lymphoma subtypes (5-year OS up to 100%). However, OS for DLBCL highly varies in the literature, ranging from 44% to 90%[4,5].
CASE DESCRIPTION
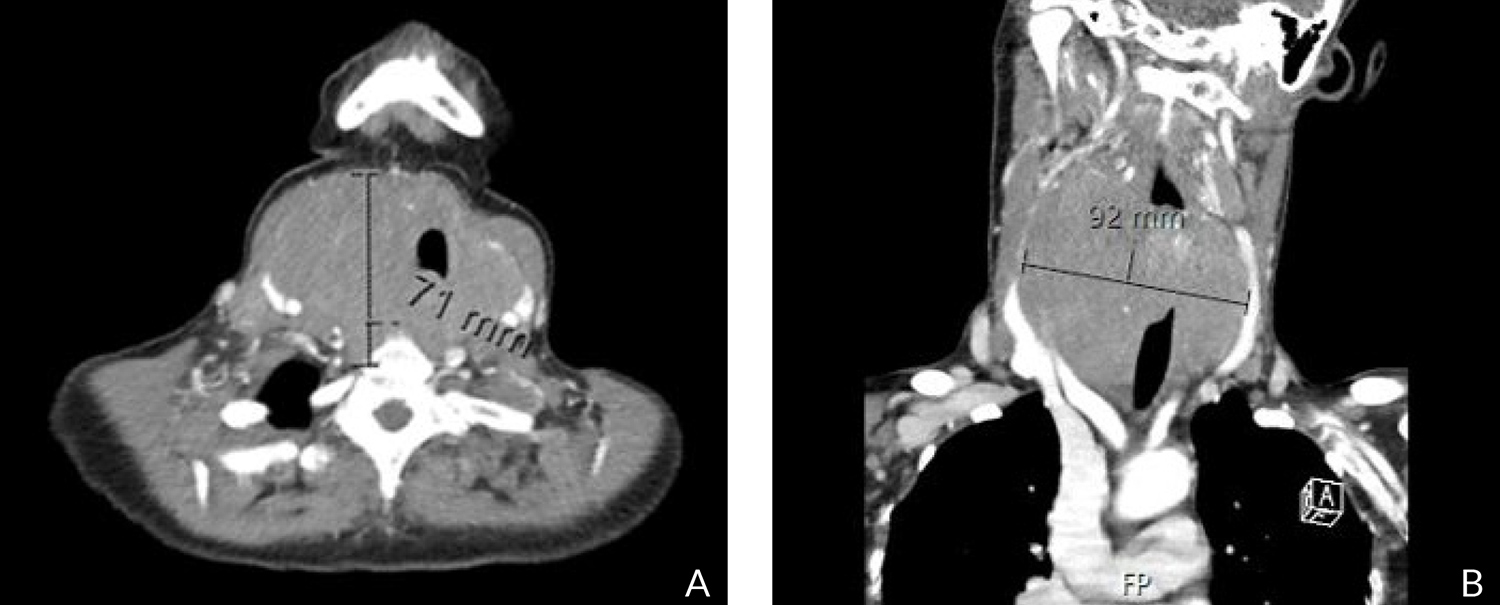
A 53-year-old woman was referred to the thyroid centre of Zuyderland Medical Centre, a large teaching hospital in the Netherlands. She presented with a rapidly growing goitre with dyspnoea, dysphagia and stridor (Fig. 1). The patient’s medical history was notable for Hashimoto’s thyroiditis. Physical examination revealed a large neck mass measuring approximately 10×10 cm. Laboratory tests showed thyrotoxicosis, due to an excessive dosage of levothyroxine. The cervical ultrasound showed a hypoechogenic lesion involving the entire right thyroid lobe as well as part of the left thyroid lobe. FNAC was performed and was suggestive but not conclusive of lymphoma. Due to severe signs of obstruction, the patient was admitted to the hospital immediately and computed tomography (CT) imaging of the neck, thorax and abdomen was performed. This showed enlargement of the thyroid gland (9.2×7.2×7.2 cm) with a left-sided deviation of the larynx and trachea (Fig. 2). Neither lymphadenopathy nor evidence of metastases was seen. After an immediate multidisciplinary team meeting with an endocrinologist, surgeon, haematologist, radiologist and pathologist, an ultrasound-guided histological biopsy was performed on the same day. High-dose prednisone (100 mg) was started while definite diagnosis was awaited. The histological biopsy showed B-cell non-Hodgkin lymphoma, stage I according to the Ann Arbor classification. Four days after her admission, R-CHOP chemotherapy (rituximab-cyclophosphamide-doxorubicin-vincristine-prednisone) was started. After three cycles of chemotherapy, the CT scan showed complete remission. The patient was treated with a total of six cycles of R-CHOP. One month after the last cycle of R-CHOP, the positron emission tomography (PET) scan showed bilateral hilar FDG-avid lymph nodes. An endobronchial ultrasound with biopsy was performed but did not show cancer recurrence. The patient has now been in remission for 12 months.
Figure 2. Computed tomography (CT) showed enlargement of the thyroid with compression of the trachea. (A) Transverse plane; (B) coronal plane.
DISCUSSION
It is important to consider PTL, in addition to anaplastic carcinoma and aggressive medullary thyroid carcinoma, in rapidly growing goitres, especially when the patient’s medical history is notable for Hashimoto’s thyroiditis. Possible complications to be aware of are tracheal invasion, superior vena cava syndrome and Horner’s syndrome[1,3]. Early recognition of PTL can often prevent surgery, which is not the preferred treatment modality. OS is higher following chemotherapy with or without radiation therapy[2].
Nevertheless, surgery is still regularly performed. Sarinah et al.[6] described 17 patients with PTL of whom 9 (53%) underwent some form of thyroidectomy. The main reasons were acute airway obstruction or severe pain (4 patients) and an unexpected diagnosis of non-Hodgkin lymphoma (5 patients) because consideration had only been given to a follicular malignancy or diagnoses had been missed with FNAC or open biopsy. This shows the importance of awareness of PTL and of obtaining a correct diagnosis before deciding on surgical intervention. Despite contemporary techniques, such as flow cytometry, immunoperoxidase studies and vectorette polymerase chain reaction to distinguish DLBCL from Hashimoto’s thyroiditis, misclassification of lymphomas is still a problem. With FNAC, even with the addition of these contemporary techniques, more than 10% of PTLs remain undiagnosed[7]. Therefore, it is important to perform a histological biopsy in rapidly growing goitres.
Finally, there are non-surgical treatment modalities for compression symptoms. Lymphomas are known to be responsive to corticosteroids and methylprednisolone rapidly improved dyspnoea, dysphagia and intermittent stridor in patients with PTL[8]. This beneficial effect was also seen in the patient presented here. Chemotherapy and/or radiation therapy will eventually relieve symptoms as well but can first exacerbate symptoms due to tissue oedema. In addition, tracheal stenting could be a less invasive and quick option, although this has only been described for thyroid-related upper airway obstruction in general, and not for PTL specifically[9]. If surgery is nevertheless necessary to relieve compression symptoms, the risk of complications appears to be low in experienced centres[10].