ABSTRACT
Behçet’s syndrome is a complex vasculitis involving vessels of all sizes. The typical clinical presentation consists of recurrent oral ulcers associated with genital ulcers, and/or intra-ocular inflammation and/or cutaneous lesions. It may also involve the joints, central nervous system, cardiovascular system and gastrointestinal tract. Muscle involvement associated with Behçet’s syndrome has been rarely described. We here report two cases of muscular manifestations in the setting of Behçet’s syndrome with specific gastrocnemius muscle involvement.
LEARNING POINTS
- Behçet’s syndrome (BS) is a vasculitis involving vessels of all sizes with multi-organ involvement.
- Myositis is a rare manifestation in the setting of BS.
- Musculoskeletal symptoms should be investigated in patients with BS.
KEYWORDS
Behçet’s syndrome, myositis, muscle
INTRODUCTION
Behçet’s syndrome (BS) is a complex vasculitis involving vessels of all sizes. The typical clinical presentation consists of recurrent oral ulcers associated with genital ulcers, and/or intra-ocular inflammation and/or cutaneous lesions. It may also involve the joints, gastro-intestinal tract, and the cardiovascular and central nervous systems[1–3]. The diagnosis can be delayed or hampered by the lack a biological marker or specific histopathological pattern[4]. Muscular involvement has been rarely described in BS. We here report two cases of muscular manifestations in the setting of BS with specific gastrocnemius muscle involvement.
CASE DESCRIPTIONS
First Case
A 25-year-old Caucasian man with Belgian ancestry presented at the internal medicine department with a 4-month history of pain in the right thigh. He had chronic oral ulcers and acneiform lesions and was a non-smoker. He had previously been diagnosed with deep vein thrombosis (DVT), pulmonary embolism, and an intracardiac thrombus in his right ventricle, later confirmed after cardiac surgery. Microbiological and biological investigations (autoimmunity, immunoelectrophoresis, serologies, bone marrow aspiration, anticardiolipin and antiphospholipid antibodies, and other coagulation investigations) had all been negative. He later developed unilateral uveitis. The patient had been diagnosed with Behçet’s syndrome (BS) based on the 2013 criteria from the International Criteria for Behçet’s Disease (ICBD)[1].
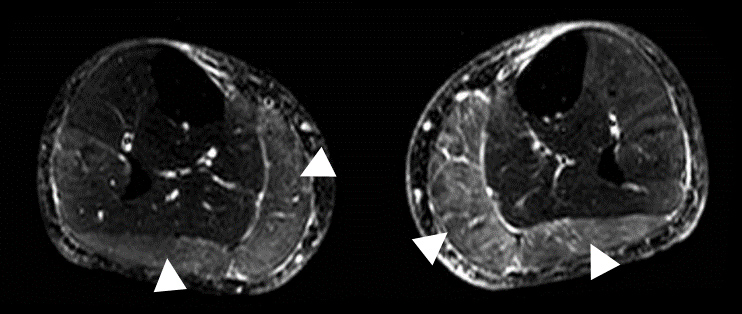
The patient developed pain with swelling of the right thigh and claudication of the lower right limb if he walked any distance. Clinical examination showed symmetrical calves but asymmetrical thighs. The neurological examination was normal with no limitation in walking a short distance. No rash had been observed. At this time, treatment consisted of azathioprine, methylprednisolone 6 mg a day, dabigatran, lisinopril, furosemide and pantoprazole. Doppler ultrasonography excluded DVT recurrence. However, MRI of the lower limbs showed hyperintensity of both gastrocnemius muscles on spectral presaturation with inversion recovery (SPIR) sequencing (Fig. 1).
Figure 1. SPIR-weighted MRI images showing hyperintense signals in the gastrocnemius muscles of both legs (white arrowheads)
Given these results, we increased the corticosteroid dosage. After 2 months, the pain resolved and long-distance walking had significantly improved. A new MRI investigation showed normal signals in the lower limbs on SPIR sequencing. We diagnosed inflammatory myopathy of the right lower limb, which responded to corticosteroids. The patient has not relapsed.
Second Case
A 29-year-old Caucasian man of Bulgarian ancestry presented with chronic pain in both legs with acute pain in his left leg. He was a non-smoker. The pain was irregular, sometimes occurred at night, and affected either one or both legs. It was relieved with paracetamol but not with non-steroidal anti-inflammatory drugs (NSAIDs). The patient did not have any relevant medical history. Anamnesis revealed frequently recurring oral ulcers.
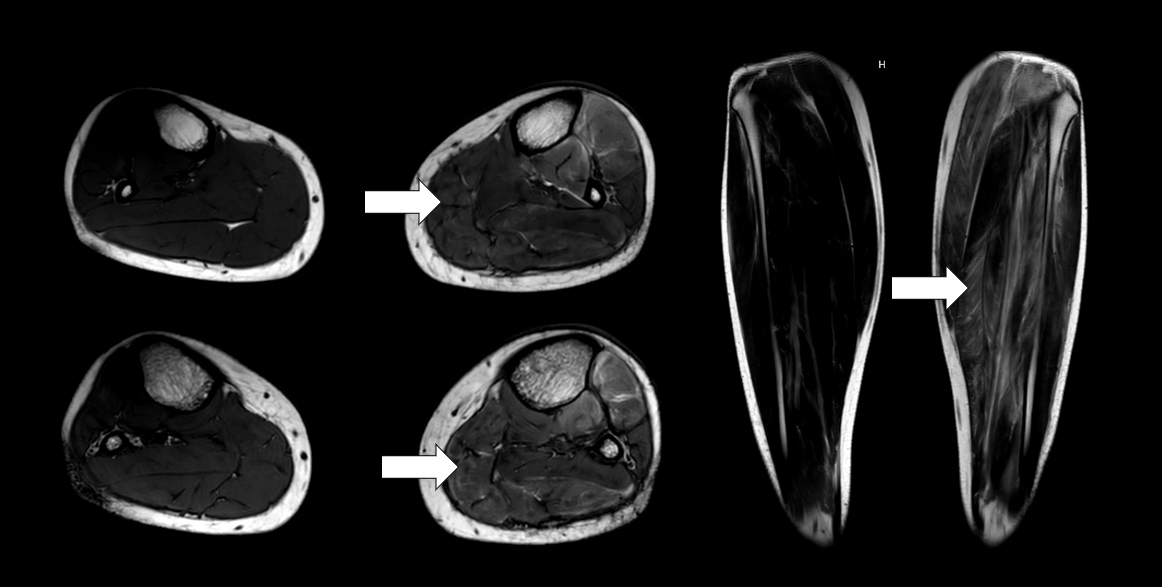
Physical examination showed folliculitis-like lesions on the chest. The left leg was diffusely painful on palpation. No skin rash was present. Investigation showed elevated inflammatory parameters with normal blood levels of creatine phosphokinase (CPK) and lactate dehydrogenase. Auto-immune serological tests including a myositis auto-antibody panel were all negative, as was a large panel of infectious serological tests. DVT was ruled out. Electromyography indicated a myogenic pattern. MRI of both legs revealed T2 hyperintensity in all muscles of the left leg and particularly in the gastrocnemius, consistent with myositis (Fig. 2). A biopsy of the same muscle showed the presence of aspecific myositis characterized by focal muscle necrosis associated with macrophage involvement, without signs of vasculitis.
Figure 1. T2-weighted MRI images revealing an enhanced signal in the posterior compartment of the left leg (white arrows)
The pain and the folliculitis responded immediately to methylprednisolone at an initial dose of 64 mg/day, which was slowly decreased to 8 mg/day. After 9 months of treatment with methylprednisolone, pain reoccurred without evidence of DVT on Doppler ultrasonography. Azathioprine was then given and stopped after a year. The patient has not relapsed since.
DISCUSSION
Diagnosis of BS in the two reported cases was based on the ICBD[1]. The first patient had vascular, ophthalmic and cutaneous involvement. The second met the criteria for oral and skin involvement, and so was considered to have possible BS. Muscle involvement in BS has been rarely described. It mostly affects the lower limbs and presents as pain associated with swelling of the affected muscle[5–10]. However, some cases have oculomotor muscle involvement only[11,12]. Both of our patients also presented with pain localised to the lower limbs.
Laboratory findings in most cases show elevated C-reactive protein (CRP) and/or an erythrocyte sedimentation rate (ESR) with surprisingly normal CPK levels[5–8,10]. Only our second case had elevated CRP and ESR. One case reported in the literature had elevated CPK levels, with a more severe clinical presentation and more diffuse muscle involvement[9].
In our patients, MRI findings were consistent with myositis. MRI seems to be an accurate diagnostic tool to detect myositis in BS patients[5–12]. Depending on the results, the differential diagnosis could include acute compartment syndrome or chronic exertional compartment syndrome if the symptoms are long-lasting. However, the clinical presentation was not consistent with such diagnoses in our patients[13]. The gastrocnemius muscle MRI findings in our cases were similar to those seen previously in other patients[5,8,14]. Gastrocnemius inflammation could be suggestive of myositis associated with BS.
Muscle abnormalities on histology have also been reported, but they do not seem to be specific, consisting of necrotic and/or atrophic myofibres and vasculitis[5–9]. The histological findings in our second patient showed muscle necrosis without vasculitis. This second patient also underwent electromyography which described a myogenic pattern. A denervation pattern on electromyography was reported in another case with muscular involvement[6].
Good response to corticoids has also been seen, with one report mentioning the use of azathioprine as a corticoid-sparing treatment[5,8]. Surprisingly, our second patient reported no response to NSAIDs. He was treated for a year with azathioprine without relapse, while our first patient had already been treated with azathioprine when myositis occurred.
In conclusion, myositis is a rare manifestation associated with BS. Other causes of myositis should be excluded as well as DVT, which should be considered first in case of swelling of the thigh in a patient with known BS. BS-associated myositis responds well to corticosteroids but we do not know if a corticosteroid-sparing treatment is needed. Our two reported cases highlight the involvement of gastrocnemius muscles as described by other authors, indicating that this localization could be preferential in the setting of BS.