ABSTRACT
Angina bullosa haemorrhagica (ABH) is a disease of unknown cause that occurs most frequently in middle-aged and older adults and is characterized by the destruction of blood vessels in the submucosal layer of the middle pharynx and larynx centred on the soft palate, resulting in the formation of haemorrhagic blisters. It usually resolves within a day and heals without scarring within about a week. No treatment is necessary. However, cases of airway obstruction due to haematemesis have been reported, and this potential risk should be considered when tracheal intubation or upper gastrointestinal endoscopy is being performed. In this report, we describe the case of a 50-year-old man who developed a haematoma in the pharynx following upper endoscopy, which spontaneously ruptured and healed, leading to the diagnosis of ABH. The main purpose of this case report is to remind the reader that ABH improves without treatment, thus eliminating the need for unnecessary examination, and that there is a risk of airway obstruction depending on the site of the lesion.
LEARNING POINTS
- The key to the diagnosis of angina bullosa haemorrhagica (ABH) is a history of acute haemorrhagic vesicles caused by an external stimulus such as food or intubation, which resolve without scarring within a week or so.
- ABH can occur at any oropharyngeal site, but its occurrence in the pharyngeal region raises the risk of airway obstruction due to haematemesis.
KEYWORDS
Angina bullosa haemorrhagica, fried foods, pharyngeal haemorrhage
INTRODUCTION
Angina bullosa haemorrhagica (ABH) has no known aetiology but can be caused by irritation to the oropharynx in the absence of underlying diseases such as abnormal blood coagulation, blistering or immune abnormalities; it heals spontaneously without scar formation in about 1 week. It can occur at any oropharyngeal site, but its occurrence in the pharyngeal region raises the risk of airway obstruction due to haematemesis.
CASE DESCRIPTION
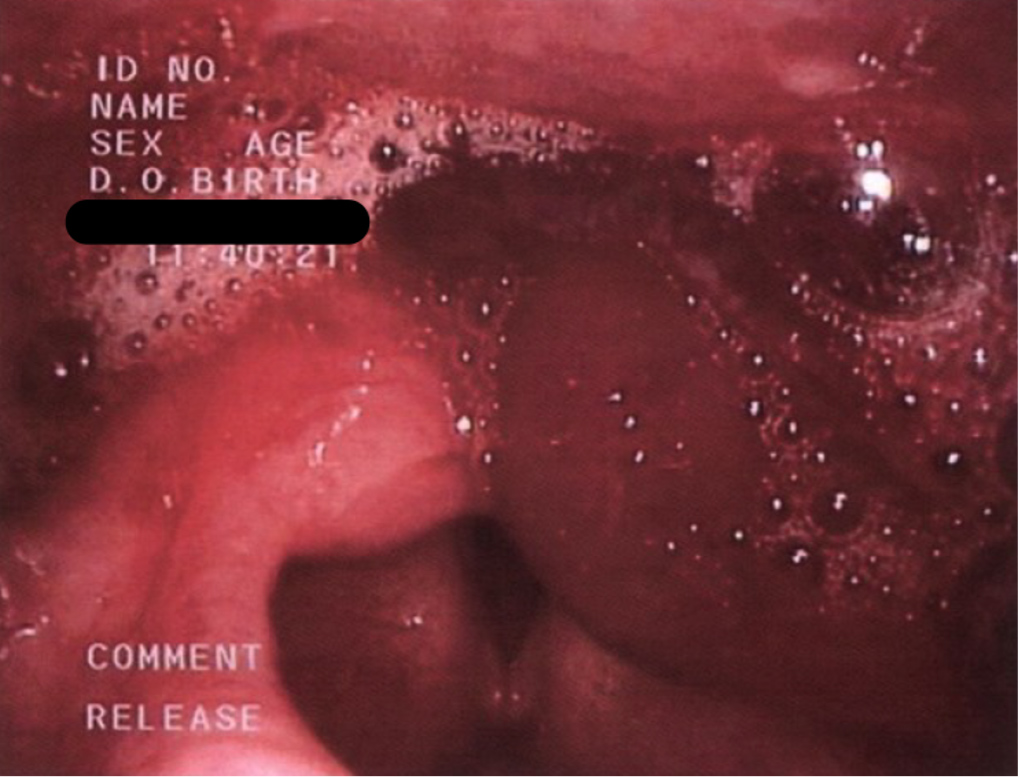
A 50-year-old man presented with a complaint of bleeding within the oral cavity. For the preceding 20 years, he had experienced episodes of pharyngeal haemorrhage immediately following the consumption of fried foods, such as pork cutlets, leading him to abstain from such items. One month before his visit, laryngoscopy had been performed to investigate haematemesis, which revealed a haematoma in the pyriform fossa and laryngeal region (Fig. 1). This haematoma resolved within a few days without intervention, but the patient was referred to our department for further investigation of the recurrent pharyngeal haemorrhage. No notable medical or familial history was reported. No abnormalities were identified upon initial examination of the oral cavity. However, immediately following the consumption of grilled dumplings for lunch, a 17×18 mm haematoma was discovered on the right side of the pharynx (Fig. 2). General blood work and coagulation test results were within the normal range. ABH was diagnosed based on the repeated occurrence of haematomas upon physical stimulation.
Figure 1. A haematoma observed in the pyriform fossa and larynx during investigatory laryngoscopy for haematemesis
Figure 2. A haematoma on the right pharynx immediately following grilled food consumption
DISCUSSION
ABH, a disorder of obscure aetiology that is prevalent among middle-aged individuals, is characterised by disruption of blood vessels within the submucosa of the oropharynx and larynx, primarily the soft palate, resulting in the formation of haemorrhagic bullae[1]. It manifests spontaneously following physical stimulation. The haematemesis typically resolves within a day, while the haemorrhagic bullae heal without scarring within approximately 1 week. Prevalence is unknown, and relapse has been reported in 62% of cases[2]. There is no gender difference, it is more common in middle-aged people, and the median age of onset is 55 years[3]. Physical or thermal stimuli such as hot drinks, dental procedures, dental anaesthesia, cigarettes, coughing or sneezing, may trigger ABH. In this case, it was caused by hot fried food and endoscopy. Other causes include a decrease in elastic fibres due to steroid inhalation, and vascular fragility due to diabetes and hypertension[4]. No treatment is deemed necessary. However, there have been reported cases of airway obstruction resulting from haematemesis[5], so this potential risk should be considered when tracheal intubation or upper gastrointestinal endoscopy is being performed.
Bullous pemphigoid was a possible differential diagnosis. This is a blistering disease, but in our patient the haematoma was localized in the oral cavity and appeared and regressed repeatedly without scarring. Blood tests were negative for anti-BP180 antibodies. Biopsy may be necessary in cases of probable bullous disease, but was not performed in this case. We also considered von Willebrand disease, an inherited haemorrhagic disorder. This condition causes mucosal and subcutaneous bleeding such as gingival and nasal haemorrhage, due to abnormal platelet function but does not present blood blisters. In addition, blood counts were normal and no coagulation abnormalities were observed, so disseminated intravascular coagulation (DIC) and immune thrombocytopenia (ITP) were also ruled out.
Most blisters heal spontaneously and do not require treatment. It is reported that gargling with 0.25% or 0.12% chlorhexidine gluconate, as well as the administration of symptomatic anti-inflammatory drugs and antibacterial drugs to prevent secondary infection, are also effective[2]. In rare cases, airway obstruction due to increased blood blisters may occur, requiring surgical drainage. The patient in this case had spontaneous remission without treatment, and has not relapsed for more than 1 year since his last visit to our department by avoiding fried food.
CONCLUSION
ABH is a rare and under-reported disease. The key to diagnosis is a history of acute haemorrhagic vesicles caused by an external stimulus such as food, which resolve without scarring within a week or so. Although the condition is benign, patients should be aware that endoscopy and intubation procedures can cause haemorrhagic vesicles, which may pose a risk of airway obstruction depending on the site.