ABSTRACT
This report describes a rare case of oligometastatic renal disease in a 69 year-old Caucasian male with non-small cell lung cancer (NSCLC). Diagnosed with Stage IIIb, NSCLC he completed chemoradiotherapy followed by 1 year of immunotherapy. Surveillance CT scans after nearly three years showed an ill-defined lesion in the left kidney.
Biopsy results were consistent with metastasis from the known lung carcinoma. Following neo-adjuvant Pembrolizumab (200mg, q3w), the patient underwent a left radical nephrectomy, without complications. One year post-operatively, CT of the thorax, abdomen and pelvis (TAP) did not identify any recurrence.
Renal metastases were historically demonstrated predominantly by autopsy studies[1]. Any mass manifesting in the kidney in the context of previous NSCLC warrants comprehensive investigations. The combination of immunotherapy followed by definitive treatment appears to be a promising management strategy[2]. With regards to local curative options, the advantages and disadvantages of surgery and radiotherapy have been well described[3-4].
LEARNING POINTS
- With improved treatment strategies for advanced malignancies, rare cases will continue to emerge and thus, maintaining a high index of suspicion is fundamental
- This case demonstrates that immunotherapy increases the efficacy of definitive treatment
KEYWORDS
Oligometastatic renal disease, immunotherapy, squamous NSCLC, nephrectomy
CASE PRESENTATION
A 69-year old Caucasian male, ex-smoker of 40 years with a 10-pack year history, was referred by his general practitioner for a chronic cough and hemoptysis. Initial chest X-ray showed a right upper lobe collapse. A computer tomography (CT) of his thorax later confirmed this but also revealed a probable right sided bronchogenic cancer, associated with local lymphadenopathy. A further positron emission tomography (PET) CT demonstrated a central right upper lobe 18F-fluorodeoxyglucose (FDG) avid tumour with bronchial obstruction and extension into the main stem bronchus with FDG avid ipsilateral, mediastinal and hilar nodes (N2). No extra-pulmonary disease was identified at this time.
Subsequent bronchoscopies provided a histological diagnosis of squamous cell carcinoma with the immunohistochemical staining of PD-L1 being more than 50%. The official diagnosis was Stage IIIb, locally advanced, unresectable non-small cell lung cancer (NSCLC). The patient went on to receive 6 cycles of weekly intravenous Carboplatin (area under curve (AUC) = 2) and intravenous Paclitaxel (50 mg/m2) with concurrent radiotherapy. Post treatment restaging CT scan showed complete response of the right upper lobe lesion with no distal metastasis. The patient then received 12 months of intravenous Durvalumab (10 mg/kg, q2w).
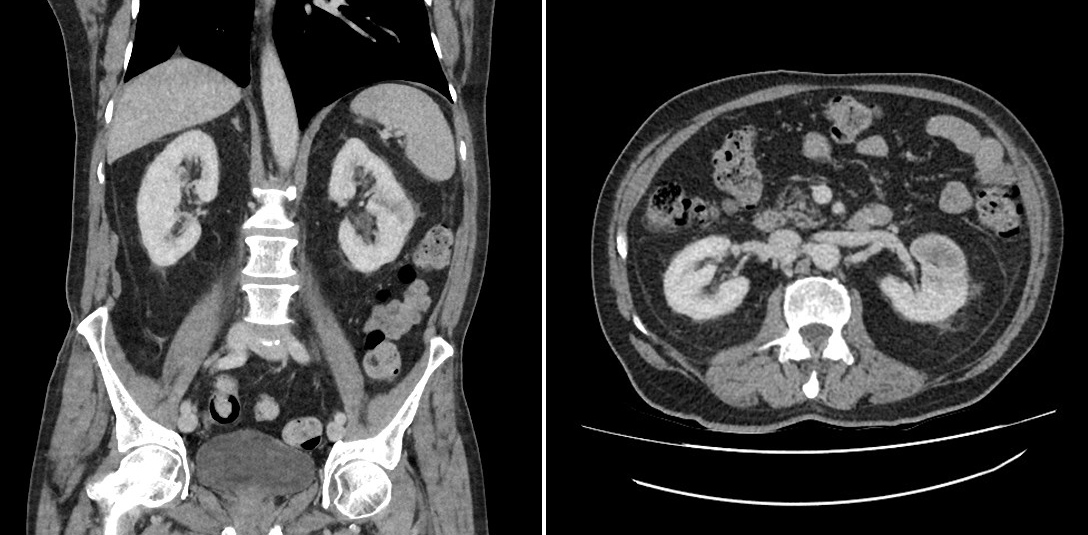
After a disease-free interval of 2 years and 9 months, surveillance CT of the thorax, abdomen and pelvis (TAP) showed an ill-defined hypodense material in the interpolar region of the left kidney despite the patient being asymptomatic (Fig. 1). Magnetic resonance imaging (MRI) of his brain was negative for metastasis. CT guided biopsy was consistent with metastasis from the known bronchogenic squamous cell carcinoma. The patient was commenced on intravenous neo-adjuvant Pembrolizumab (200 mg, q3w) and underwent a left radical nephrectomy without complications. Post-operative pathological diagnosis of squamous cell carcinoma was consistent with the initial renal biopsy results. One year post-operatively, the patient remains on ongoing surveillance, is doing well and routine CT TAP did not identify any signs of recurrence.
Figure 1. Computer tomography of patient's abdomen showing left renal metastasis, Coronal and Axial views
DISCUSSION
Lung cancer has been a reportable disease for more than a hundred years. Despite the kidney being an exceedingly uncommon site of metastasis, it is not unreasonable to suggest that any mass manifesting in this organ in the context of previous NSCLC warrants a full battery of investigations to exclude the possibility of this exceedingly rare occurence. In fact, in isolated renal metastasis, the most common primary tumor site is the lung[1]. The kidneys are the 2nd most “common of the uncommon” metastatic sites of NSCLC. By virtue of being uncommon, renal metastases are an independent poor prognostic factor[5]. In many ways, our patient had several factors in favour of a satisfactory outcome from the aggressive multimodal approach that was initiated for his oligometastatic disease. These factors include good control of the primary site, a confirmed solitary metastatic disease, an Eastern Cooperative Oncology Group (ECOG) score of 1, a metachronous lesion and a disease-free interval of more than 2 years[6].
In comparison to previously described cases, our patient had a more advanced stage of malignancy[7]. He remains in complete remission a year following treatment with neoadjuvant immunotherapy followed by surgery. A combination of immunotherapy followed by definitive treatment appears to be a promising strategy[2].
However, careful consideration of the tumor biology and the benefits of surgical intervention as a curative option must be weighed against the risk of aggravating the expansion of metastases[3]. Verma et al.[4] reported early tumor control, ability to spare surrounding tissues and symptomatic relief in patients with renal metastasis who received stereotactic body radiation therapy (SBRT). Furthermore, radiation therapy has the advantage of inducing a systemic antitumor response: the abscopal effect[8]. At present, there are no known prospective randomized studies comparing surgery versus SBRT.
CONCLUSION
With advancements in treatment for lung cancer leading to improved control of the primary tumour, it is reasonable to suggest that unique presentations as outlined in this case will continue to be reported in the literature. Thus, the possibility of a solitary metastatic renal deposit should readily be considered upon detection via radiological imaging. As more of these cases emerge, acknowledging “uncommon” diseases may not be as unconventional as previously thought. This should prompt further research to determine the most beneficial therapeutic option going forward.