ABSTRACT
A nuclear protein in testis (NUT) midline carcinoma arises from squamous cells and is often located in the head, neck, and lungs. This report focuses on the negative p63 mutation and older age at the diagnosis of a NUT carcinoma, which has significant prognostic implications. A 62-year-old patient presented initially with a three-year history of recurring frontal headaches, intermittent nasal bleeding, and a sensation of a nasal cavity mass. An incisional biopsy revealed a poorly differentiated NUT carcinoma in the left maxillary sinus. A functional endoscopic sinus surgery was performed, but the cancer recurred. As a result, a total maxillectomy was performed, and the patient was declared cancer-free with no evidence of residual disease. This is a rare instance of a p63-negative midline NUT cell carcinoma (NCC) in an elderly patient, which could potentially contribute to a more favourable prognosis and longer survival compared to other reported cases.
LEARNING POINTS
- Molecular analysis of a NUT carcinoma and age at diagnosis may serve as a potential means for predicting patient prognosis in cases of midline NCC.
- Each patient should receive careful monitoring and a personalised treatment strategy based on their molecular studies. Surgical resection, along with a combination of radiotherapy and chemotherapy, has the potential to improve overall survival rates.
- In line with the commonly observed relationship between increased p63 mutation and poorer survival rates, a negative p63 expression in squamous cell carcinomas may indicate a more favorable prognosis. This hypothesis highlights the importance of further research to validate these findings.
KEYWORDS
Cytokeratin, NUT midline carcinoma, NMC, squamous cell carcinoma, p63
INTRODUCTION
Of the various subtypes of squamous cell carcinomas, the nuclear protein in testis (NUT) carcinoma is considered to be a very rare yet aggressive subtype. The midline organs such as the mediastinum and upper aerodigestive tract provide the origin of one of its subtypes and are hence known as NUT midline carcinomas (NMC)[1]. The median age of diagnosis is 23 years. NMC features a t(15;19) chromosomal translocation causing gene suppression and undifferentiated cell proliferation. Diagnosis relies on NUTM1 gene identification via fluorescence in situ hybridisation (FISH) or reverse transcription polymerase chain reaction (RT-PCR). Unfortunately, NMC has a poor prognosis with a median overall survival of only 9 months. It has been observed that tumours larger than 5 cm have a worse prognosis compared to smaller tumours. In our case, the patient’s tumour measured 6 × 3.2 × 2.6 cm, yet her overall survival surpassed the median overall survival. On immunohistochemical staining, NMCs routinely stain positive for p63, although there have been rare cases of p63-negative NMCs. It is worth noting that an older age at presentation and a negative p63 status appear to be associated with better survival rates[2].
CASE DESCRIPTION
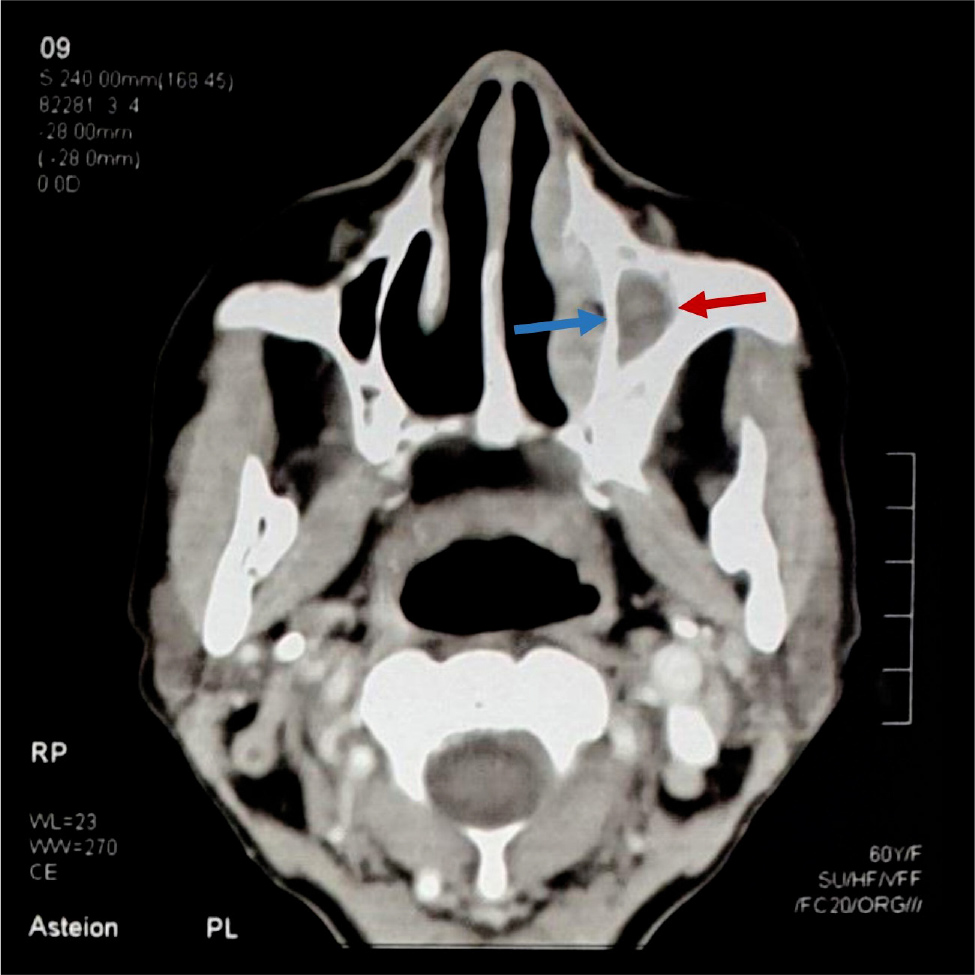
A 62-year-old woman presented with recurrent headaches and nasal bleeding for the past 3 years. She had been diagnosed with a NUT cell carcinoma (NCC) three years previously after experiencing intermittent bleeding from her left nostril and feeling a mass in her left nasal cavity for over 6 months. A CT scan showed a polypoidal mass measuring 6 × 3.2 × 6.0 cm in her left ethmoid sinus (Fig. 1). An incisional biopsy revealed polypoid fragments infiltrated by a malignant neoplasm composed of small to medium-sized cells arranged in sheets with minimal cytoplasm, mitosis, and areas of necrosis. Immunohistochemical staining showed the mass to be positive for NUT and cytokeratin (CK), and negative for p63, encoded small nuclear RNAs (EBER), p40 and insulinoma associated protein 1 (INSM-1). The definitive diagnosis at that time was a poorly differentiated NUT carcinoma. A functional endoscopic sinus surgery was performed, followed by a combination of intravenous cisplatin and 5-fluorouracil, and radiotherapy for the next 6 months.
Figure 1. Presurgical contrast-enhanced CT scan image shows soft tissue density exaggeration along the medial wall of the left maxillary sinus (red arrow) with evidence of hypertrophy of the turbinates (blue arrow)
One year later, the patient returned with a recurrence of her initial symptoms. A mass was found in her left nostril. Microscopic examination of the tissue sample revealed the presence of small to medium cells with hyperchromatic nuclei, limited cytoplasm, multiple mitoses and areas of keratinisation. Immunohistochemical staining showed that the tissue was positive for NUT and CAM 5.2, but negative for cytokeratin, p63, LCA, synaptophysin and calretinin. A cervical spine scan showed multiple small osseous lytic lesions which were suspicious for metastatic deposits. Subsequently, a medial maxillectomy and lateral rhinotomy were performed to remove the tumour while preserving normal structures.
However, two months later, the patient returned with persistent nasal obstruction and bloody discharge from the nose. A CT scan showed a 4 × 3.4 × 2.5 cm mass lesion eroding the medial wall of the left maxillary sinus (Fig. 2). After further examination and immunohistochemical staining, a diagnosis of recurrent NCC was confirmed. The patient was then scheduled for a total maxillectomy, which took place three months later.
Figure 2. The CT scan revealed a soft tissue mass that completely obstructed the left nasal cavity with a complete loss of lucency of the left maxillary sinus, causing erosion of the medial wall of the maxillary sinus (red arrow). However, the nasal septum is intact.
DISCUSSION
The World Health Organization (WHO) has classified the NUT cell carcinoma as a carcinoma with a t(15;19) translocation, with a BRD4-NUT fusion product formed in 66% of cases from the fusion of the BRD4 (19p13.1) and NUT (15q14) genes. NCC can affect people of any age; once described as a paediatric disease, according to literature its presence has even been detected in patients as old as 78 years[1]. The disease has a predilection for the female gender, and young age[1]. NCC can occur in a variety of anatomical places such as the region of the head and neck, and the mediastinum, but most commonly occurs in the midline, in a variant known as a NUT midline carcinoma (NMC). In the head and neck area, 73.4% of NCCs occur in the sinonasal tract[1]. Patients usually present with a rapidly enlarging nasal mass and nasal-related symptoms such as rhinorrhoea, epistaxis, nasal obstruction and facial pain.
The only established positive prognostic factor in NMC patients is the presence of NSD3 or BRD3 NUT positive NMC compared to BRD4 NUT. Recurrences in NMC are quite common and tend to occur frequently if the patient survives for longer than the prognosis allowed. McLean-Holden et al. report a case where, like our case, the patient experienced a recurrence of the tumour twice. However, their patient experienced recurrences at 56 months after the initial resection and 59 months following the second resection[4]. Our patient experienced recurrences at much earlier dates, already experiencing two recurrences within two years of the initial diagnosis. Surgical resection had negative margins, and combination radiotherapy and chemotherapy had been related to an enhancement in the progression-free survival rate and overall survival rate compared to management involving just radio-chemotherapy[4].
At first glance, midline NCCs are indistinguishable from poorly differentiated squamous cell carcinomas due to their non-specific morphologic features[1]. Immunohistochemical staining helps to differentiate between the two; NCC is commonly positive for cytokeratin, p63 and CD34. However, in our case, the midline NCC tested negative for p63, which is a unique finding as there have been only a few previous cases with negative p63 staining. For squamous cell carcinomas of the head and neck, a statistically significant relationship between increased p63 expression and poorer survival rates has already been noted[3]. This may explain why our patient, with a p63-negative NMC, has a better prognosis and survival compared to other cases in the literature. Another case involving a p63-negative pulmonary NUT carcinoma has also been reported in an elderly patient, showcasing atypical clinical features (such as age, size and location) and a less severe disease presentation[5]. This further emphasises the importance of maintaining a high level of suspicion for NUT carcinoma regardless of age, clinical presentation, tumour location or p63 expression[5].
Additionally, it has been observed in the literature that older age at presentation is associated with better survival rates. For instance, a patient diagnosed at 48 years had double the survival rate (16 months) compared to a patient diagnosed at 26 years (8 months), while a patient diagnosed at 33 years had a survival rate in between (11 months)[2]. Our case describes an elderly patient with a NUT carcinoma who has a survival rate of over 24 months.
The role of p63 gene mutation in the long-term survival of the patients still remains uncertain and can guide research into further confirming its role in the prognosis of NUT carcinoma and relating it to the survival of patients.
CONCLUSION
Based on the available data, we can hypothesise that an increased age at presentation and a negative p-63 in NUT carcinomas may indicate a milder form of the disease and improved survival rates. However, further research at a molecular level is required to conclusively validate our hypothesis.