ABSTRACT
We describe a case of ventricular fibrillation occurring in a patient with multi-vessel coronary spasm after the initiation of an oral beta-blocker. A 56-year-old man began to experience chest discomfort and his computed tomography revealed intermediate coronary stenoses. He was administered medications including an oral beta-blocker but suddenly collapsed while walking 4 days later. An automated external defibrillator detected ventricular fibrillation and delivered successful electrical cardioversion. An acetylcholine provocation test after stabilization of the status revealed triple-vessel coronary spasm. Beta-blockers may provoke exacerbation of coronary spasm and result in lethal arrhythmia.
LEARNING POINTS
- Beta-blockers which have a vasoconstrictive effect may occasionally provoke exacerbation of coronary spasm.
- Coronary spasm should be considered as a cause of lethal ventricular arrhythmia or cardiac arrest.
KEYWORDS
Coronary spasm, ventricular fibrillation, beta-blocker, acetylcholine provocation test.
INTRODUCTION
Beta-blockers have a vasoconstrictive effect and may provoke exacerbation of coronary spasm[1]. It is known that coronary spasm can cause serious arrhythmias and consequently sudden cardiac death[2]. We herein describe a case of ventricular fibrillation occurring in a patient with multi-vessel coronary spasm 4 days after the initiation of an oral beta-blocker.
CASE REPORT
A 56-year-old man with a history of dyslipidaemia began to experience chest discomfort on effort and at rest. He presented to a local hospital where coronary computed tomography revealed intermediate stenoses in the mid portion of the left anterior descending artery (LAD) and the first diagonal branch. The patient was prescribed medications including low-dose aspirin, a statin and a beta-blocker (atenolol 25 mg once daily), but his symptoms worsened.
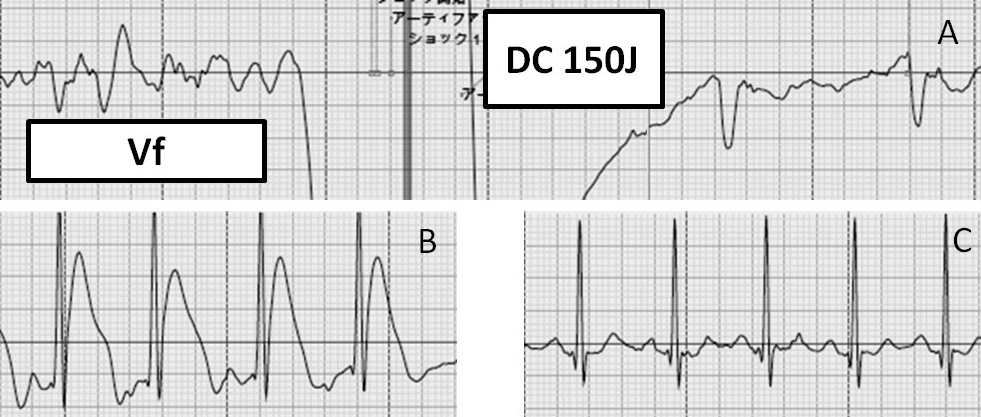
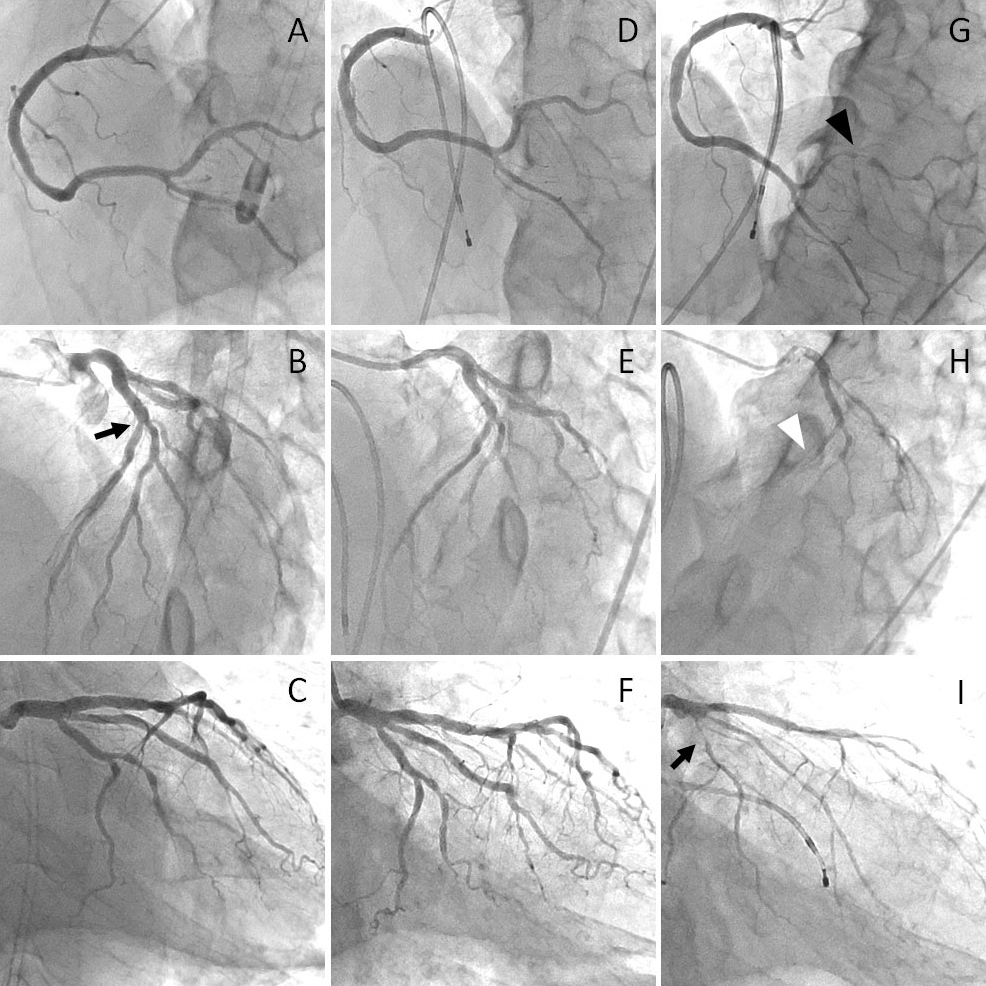
Four days later he took his medications and went shopping on foot. At 10 am, he suddenly collapsed while walking. Cardiac massage was immediately performed by bystanders and after 5 min of resuscitation effort, an automated external defibrillator (AED) was attached. It detected ventricular fibrillation and delivered a successful electrical cardioversion (Fig. 1A). The AED electrocardiogram (ECG) record just after successful cardioversion showed ST-segment elevation (Fig. 1B), which disappeared promptly (Fig. 1C). After the return of spontaneous circulation, the patient was brought to the emergency department of our hospital.
DISCUSSION
Beta-blockers reduce heart rate and contractility, resulting in relief of myocardial ischaemia. However, blockade of the vasodilatory β2-adrenergic effect even with β1-selective agents[3] and relative enhancement of the vasoconstrictive α1-adrenergic effect[1] can result in exacerbation of coronary spasm and provoke lethal arrhythmia. In this case, the patient had experienced ventricular fibrillation 4 days after the initiation of an oral β1-selective adrenergic blocker, and was ultimately diagnosed as having multi-vessel coronary spasm. The fact that multi-vessel spasm was provoked by intracoronary injection of low-dose acetylcholine indicates that this patient’s baseline coronary artery tone may be high. To our knowledge, there are few cases of the initiation of oral beta-blocker therapy resulting in ventricular fibrillation in patients with coronary spastic angina.
Coronary spasm can cause critical ischaemic heart disease. In particular, multi-vessel spasm is often complicated by lethal ventricular arrhythmias[4], similar to our case. A previous study reported that reperfusion after coronary spasm, rather than coronary spasm itself, correlated with the onset of ventricular arrhythmia in some cases[4]. Those patients may not be diagnosed as having coronary spasm following emergency coronary angiography just after resuscitation. Physicians should perform a spasm provocation test after the patient has stabilized and emergency coronary angiography had not revealed any likely cardiac lesions, because coronary spasm was detected in 11% of patients who survived cardiac arrest without structural heart disease[5]. Coronary spasm is a more common cause of lethal ventricular arrhythmia or cardiac arrest than one might expect.