ABSTRACT
Giant cell arteritis or temporal arteritis is an inflammatory condition affecting medium to large sized vessels, particularly the cranial arteries. A 76-year-old man with no significant past medical history presented to the emergency department with a 3-week history of diffuse headaches associated with fever, loss of appetite, weight loss and general malaise. A CT scan of the brain showed bilateral shallow chronic low density subdural haematomas. A complete laboratory panel was unremarkable except for a raised erythrocyte sedimentation rate and elevated C-reactive protein. A transthoracic echocardiogram and CT scan of the body were unremarkable. MRI of the brain confirmed bilateral old subdural collections and showed marked vessel wall enhancement in the frontal branches of the left superficial temporal artery. A left temporal artery biopsy confirmed giant cell temporal arteritis. We speculate that a vasculitic process in the small subdural arteries may have contributed to our patient’s spontaneous subdural haematomas.
LEARNING POINTS
- A contrast-enhanced T1 axial fat-suppressed MRI of the brain is a non-invasive modality of diagnostic value in giant cell arteritis (GCA); increased access to high resolution MRI technology may reduce the requirement for invasive temporal artery biopsy in the future.
- Subdural hematomas may be of arterial origin; GCA has been reported in association with subdural hematomas but causation is not proven.
- GCA must be suspected in patients presenting with headaches and raised inflammatory markers even in the absence of classic features or dual pathology as failure to recognize and treat promptly could lead to permanent visual loss.
KEYWORDS
Giant cell arteritis, subdural hematoma, arterial origin.
INTRODUCTION
We present the case of a 76-year-old Irish man who attended the emergency department complaining of having headaches for the last 3 weeks. He had no previous history of headaches. His symptoms initially started after he had used a new treadmill and presented as gradual occipital headaches that eventually spread to the frontal area. The headaches were described as dull, diffuse, constant and throbbing in nature with transient relief obtained with administration of paracetamol. The headaches were associated with fevers, sweats, fatigue and a decreased appetite. The patient had attended his general practitioner at the end of the second week and was given an oral antibiotic with no improvement. The patient then decided to visit the emergency department.
A detailed history was taken in which our patient denied any visual disturbance, neck stiffness, rash, disorientation, dizziness, tinnitus, aches/pains, weakness or jaw pain. He denied temporal headache or tenderness. He also denied any head injury, trauma or loss of consciousness.
He had no significant past medical history apart from right-sided glaucoma and no regular medication use, and denied substance abuse. He had no significant family history. He was an active retired factory worker who lives at home with his wife. He is a lifelong non-smoker and denied excessive alcohol intake.
Full examination was unremarkable apart from a temperature of >38°C, a soft pan-systolic murmur and a decreased non-tender left temporal pulse. A laboratory panel was unremarkable apart from raised inflammatory markers and neutrophil leucocytosis (Table 1).
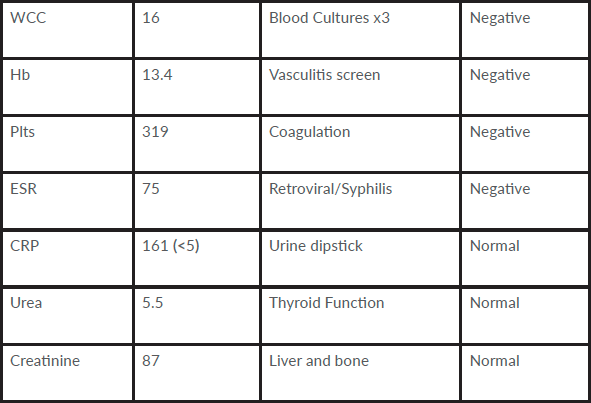
CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; Hb, haemoglobin; Plts, platelets; WCC, white cell count.
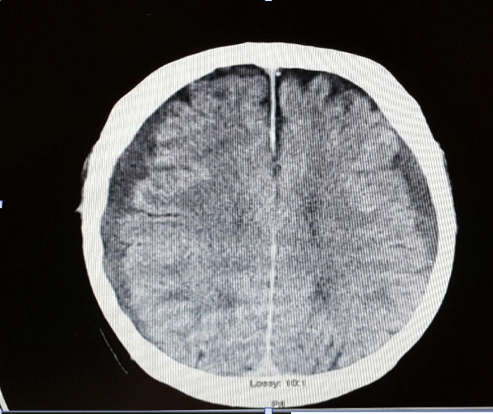
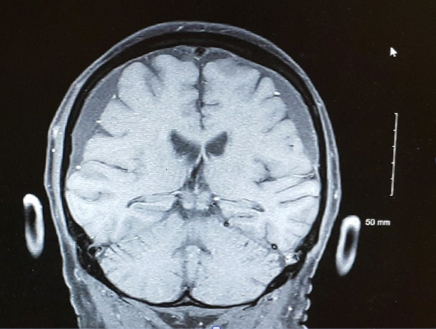
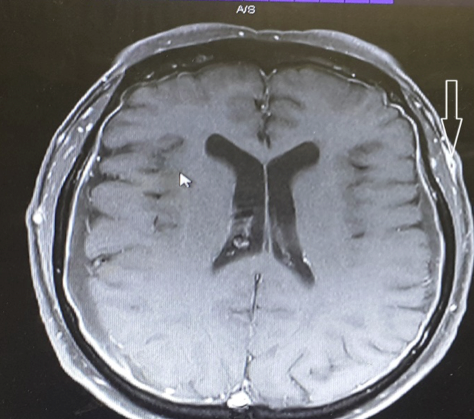
AECG revealed a normal sinus rhythm. A transthoracic echocardiogram showed normal cardiac function and valves. A CT scan of the brain showed bilateral shallow, chronic, low density, symmetrical subdural hematomas (Fig. 1). Following a radiology multidisciplinary discussion, the possibility of an infected haematoma was considered but it is rare and so was deemed unlikely. Contrast enhanced MRI of the brain demonstrated large bilateral chronic subdural collections. Meningeal enhancement was noted and thought to be non-specific in the setting of chronic haemorrhage and infection. There was also enhancement of the walls of the frontal branch of the superficial temporal arteries, especially on the left, on axial fat-suppressed T1 MRI (Fig. 2a,b). CT scans of the thorax, abdomen and pelvis were unremarkable.
Giant cell arteritis (GCA) was considered likely, with immediate commencement of high dose prednisolone (60 mg once a day).
Ophthalmology review showed no abnormal ophthalmic findings. Left temporal artery biopsy confirmed histological features of temporal arteritis.
DIFFERENTIAL DIAGNOSIS
- Infection (abscess, meningitis)
- Vasculitic (temporal arteritis, systemic lupus erythematosus)
- Systemic (drugs, systemic infections)
- Ears/sinus (sinusitis, otitis media, mastoiditis)
- Haemorrhage (subdural, intracerebral)
- Cerebral space-occupying lesion
Figure 2a. Contrast enhanced MRI of the brain (coronal section).
Figure 2b. Left temporal artery thickening and enhancement on contrast enhanced axial T1 fat-suppressed MRI of the brain
TREATMENT, OUTCOME AND FOLLOW UP
GCA is an inflammatory condition predominantly affecting medium to large vessels, particularly the cranial arteries. Incidence increases progressively with age after the age of 50 and usually peaks in the seventh decade. The female:male ratio is 3:1 and it is more common in Northern European population[1]. As headache is a very common presentation, it is important to be vigilant and give full consideration to an appropriate list of differential diagnoses for headache particularly in the absence of the classic features of a suspected cause.
About 75% of patients with GCA will present with new onset headache, and, although frequently located in the temporal regions, it can vary in nature and location[1]. Therefore, headache which is not temporal in nature should not eliminate GCA from the differential diagnosis. GCA should be considered in a patient over the age of 50 presenting with new onset headache associated with unexplained fever, new visual disturbance or raised inflammatory markers. Failure to consider and treat GCA promptly could potentially result in irreversible blindness.
A temporal artery biopsy is the recognized gold standard for the diagnosis of GCA, although the initiation of treatment should not wait until histological confirmation[2]. Among other imaging modalities, high resolution MRI has been shown to have a sensitivity of 80.6% and specificity of 97%[3] compared with a sensitivity of 77.8% and specificity of 100% for histological methods[3]. Our patient did not have the classic tender, thickened, nodular and painful temporal arteries and the use of contrast enhanced MRI prompted us to the diagnosis of GCA which was confirmed by temporal artery biopsy.
In this case, there was no history of provoking falls, seizures, alcoholism or coagulopathy. We hypothesize that there may a link between the bilateral subdural haematomas and GCA. There have been previous case reports linking these conditions. Tomura et al.[4] and Kotani[5] reported similar cases of biopsy-proven GCA in conjunction with subdural haematomas. The mechanism for this link may be vasculitic arterial damage leading to bleeding from small subdural arteries which traverse the subdural space. Contrary to popular belief, it has been proven neurosurgically that traumatic or spontaneous laceration of cortical arteries has led to subdural haematomas, but this is rare[6]. Although these findings may be co-incidental, we speculate that a link should be considered.