ABSTRACT
Light-chain deposition disease (LCDD) is a rare monoclonal gammopathy that involves the deposition of light chains (LC) in multiple organs, leading to progressive dysfunction. The kidney is usually the most affected organ and responsible for the initial clinical manifestations. We present the case of a patient with LCDD with prominent liver involvement (marked cholestasis, hepatomegaly and portal hypertension) but with no evidence of coexisting lymphoproliferative disorder.
LEARNING POINTS
- Light-chain deposition disease (LCDD) is rare, and diagnosis can be challenging, especially in the absence of a coexistent lymphoproliferative disorder. The presence of light chains in blood or urine can be intermittent, and immunohistochemistry results of biopsy can be difficult to interpret. Hence, there is a need for a high level of suspicion in this diagnosis.
- Although renal involvement is the most classic presentation, LCDD should be suspected when there is multiple organ involvement, as in this case, even when renal manifestations do not dominate the clinical picture.
- Prognosis depends on the affected organs, and treatment should be started as rapidly as possible to suppress production of the clonal light-chain and halt organ damage.
KEYWORDS
Light-chain deposition; monoclonal; plasma cell
CASE DESCRIPTION
We present the case of a 60-year-old Caucasian man admitted to our unit with a history of generalized weakness, cough and progressive exertional dyspnoea progressing over the previous 2 months, with anorexia and postprandial fullness on the previous days.
Upon observation, the patient was oriented, with no signs of distress. He had no palpable lymphadenopathies or skin rash. Cardiac and pulmonary auscultation was normal. Abdominal examination showed tender hepatosplenomegaly, with a hard spleen border, with no rebound or guarding.
Laboratory studies revealed anaemia (Hb 11.3 g/dl), leucocytosis (31,300 cells/μl), renal insufficiency (urea 93 mg/dl, creatinine 2.7 mg/dl) and mildly elevated gamma-glutamyl transpeptidase (GGT) 90 U/l and alkaline phosphatase (ALP) 520 U/l. Chest radiography showed cardiomegaly and hilar congestion.
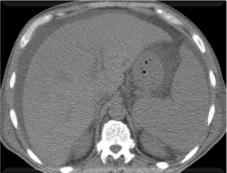
An abdominal CT scan showed an enlarged liver (20 cm in the mid-axillary line) with no focal lesions, homogeneous splenomegaly (22 cm), no biliary dilation or venous thrombosis, and small ascites (Fig. 1). Kidneys were normal.
The patient had contact with animals (dogs, pigs and cows), but denied fever, known tick bites, or consumption of untreated water or unpasteurized dairy products.
Blood, urine and sputum cultures were negative, as were serological tests for viral hepatitis, HIV, brucellosis, leptospirosis and leishmaniosis, ruling out more obvious causes of hepatosplenomegaly in this epidemiological context.
The blood smear and bone marrow biopsy were normal, with a bone marrow aspirate showing slight plasma cell elevation (6%) with 0.3% blasts. Autoimmune screening was negative. Serum protein electrophoresis and peripheral B-cell immunophenotyping were normal and no monoclonal component was detected in immunofixation. Beta-2 immunoglobulin was elevated (12.1 mg/l).
Diuresis was preserved and renal function improved during the first few days (creatinine 1.9 mg/dl), with a proteinuria of 424 mg/24 h. However, due to progressive worsening of cholestasis (maximum GGT 1032 U/l and AP 1377 U/l) and hyperbilirubinemia, a magnetic resonance cholangiopancreatography was performed, which excluded biliary tract dilations or lesions and revealed signs of portal hypertension. The echocardiogram showed moderate bi-atrial enlargement and increased echogenicity of the ventricular walls. A liver biopsy was performed, showing cholangitis with secondary sclerosis, with negative Congo red staining. A bone marrow biopsy was also negative for the Congo red stain.
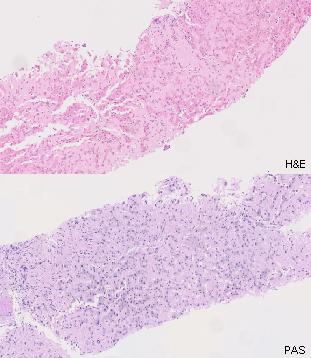
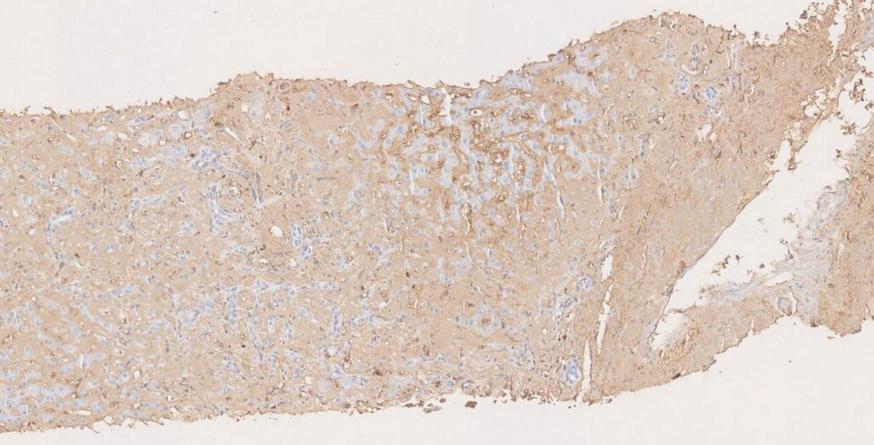
Despite the biopsy results, the apparent involvement of the liver, spleen, kidney and heart supported the suspicion of an infiltrative disease, prompting further investigation. Light chain studies were ordered, showing elevated serum kappa light chains (69.20 mg/dl; normal 0.33–1.94 mg/dl), with an elevated kappa/lambda relationship (14:18; normal 0.26:1.65). Urinary immunoelectrophoresis revealed a monoclonal component corresponding to elimination of kappa light chains. Liver biopsy was revised under this new clinical information, revealing deposits of eosinophilic amorphous material with sinusoidal distribution, with negative Congo red staining and an inconclusive immunohistochemical study with anti-kappa light chain antibodies (Figs. 2 and 3). Based on the deposit morphology and Congo red negativity, along with the elevation of serum kappa light chains and a monoclonal band, a diagnosis of LCDD was assumed.
Treatment with chemotherapy was initiated, but the patient had multiple infectious complications and died 2 months after the diagnosis.
Figure 2. Liver biopsy (HE and PAS colouration) showing deposition of amorphous, eosinophilic material, negative for Congo red staining
Figure 3. Immunohistochemistry staining for CD138, kappa and lambda light-chain antibodies
DISCUSSION
LCDD is a rare monoclonal plasma cell proliferative disorder characterized by the deposition of LC in the basement membranes, ultimately leading to organ dysfunction. The deposits are non-amyloid, do not stain with Congo red and do not exhibit a fibrillar ultrastructure[1]. Hepatic LC deposits assume a perisinusoidal distribution, as opposed to amyloid deposits, mostly in liver parenchyma[2,3].
This condition is systemic in nature, and can manifest in different organs (like the heart, liver, lung and nerves), although the main target organ is usually the kidney (with symptoms ranging from asymptomatic proteinuria to nephrotic syndrome and rapidly progressive renal impairment)[4]. Prominent involvement of other organs is less common. In our case, although there was also renal and heart involvement, the clinical picture was dominated by hepatic manifestations, which led to a wider variety of differential diagnoses. This degree of hepatomegaly, severity of cholestasis and signs of portal hypertension are not very common in LCDD[3].
About 65% of patients have an associated lymphoproliferative disorder (multiple myeloma, lymphoma, leukaemia), and up to 85% have kappa LC deposits (as opposed to amyloidosis with mainly lambda LC)[1,2]. Diagnosis can be challenging as about 60% of cases do not have a detectable serum monoclonal immunoglobulin due to kappa LC aggregation[1], detection of serum and/or urine light chains may be intermittent, and demonstration of LC deposits on biopsy may be difficult due to false-negative results even with specific antibodies[4]. The free chain kappa/lambda ratio is altered, making it a useful test[1].
The absence of evidence of coexistent lymphoproliferative disorders and of a serum monoclonal component made the diagnosis more difficult in our case, together with an initially uninformative liver biopsy, showing that correct histological diagnosis also requires a high degree of suspicion.
There is not much data on the natural history and treatment of LCDD due to its rarity. Prognosis is unfavourable, largely dependent on affected organs, and aggravated by delayed diagnosis leading to the occurrence of more advanced organ dysfunction[1]. A mean survival of 34 months has been described, but can be as low as 6 months with severe cardiac involvement or 5 months with cholestatic jaundice[2], as in our case. Treatment aims to control plasma cell proliferation, LC production and favour its catabolism, delaying or halting organ damage, and currently is largely based on multiple myeloma regimens[1,2].