ABSTRACT
Patients who survive a traumatic brain injury (TBI) can sometimes experience symptoms of excessive sympathetic discharge. Despite being known about for more than 60 years, the diagnostic criteria for this condition have only recently been defined under the name "paroxysmal sympathetic hyperactivity". Failure to recognize this syndrome leads to excessive costs, prolonged hospital stays and delayed recovery for TBI patients. This case report describes a patient whose specific rehabilitation program was affected by a failure to identify this entity, even though he presented with many of the characteristics of this condition.
LEARNING POINTS
- Fever is a common sign in hospitalized patients and can result in expensive investigations and prolong length of stay.
- It is crucial to consider paroxysmal sympathetic hyperactivity (PSH) as a cause of fever in traumatic brain injury patients (TBI).
- A delay in diagnosing and treating PSH can have devastating consequences for these patients' recovery programs.
KEYWORDS
Paroxysmal sympathetic hyperactivity (PSH), traumatic brain injury (TBI), fever, beta-blocker
CASE PRESENTATION
The authors report the case of 27-year-old male who was aphasic and tetraplegic following a traumatic brain injury (TBI) with severe right hemisphere lesions sustained in a road traffic collision. Five months after the accident, the patient was readmitted to hospital because of nosocomial pneumonia and was started on a 10-day course of the antibiotic meropenem. No pathogens were isolated from blood or sputum cultures and the patient improved clinically to be stable on air, with no respiratory symptoms and negative inflammatory markers.
Despite the apparently treated infection, the patient was still febrile with his temperature rising to 39.5°C once or twice a day with very little response to antipyretic drugs. During these episodes, the patient became tachycardic, hypertensive, tachypnoeic and sweated profusely. The patient´s mother reported that these episodes were also frequent at home and that because of them, the patient had been refused care in a specialized rehabilitation hospital as he was thought to be infectious.
A complete septic screen was performed including blood, sputum (obtained from bronchoscopy), urine and liquor samples but no bacteria, yeast or fungus were found, and no changes were seen on imaging tests. The inflammatory markers were also negative: white cell count 7,000×109/l (normal value <11,000×109/l), C-reactive protein <0.5 mg/dl (normal value <0.5 mg/dl) and erythrocyte sedimentation rate 23 mm/h (normal value <20 mm/h). Both renal and liver function were normal.
Paroxysmal sympathetic hyperactivity (PSH) was then considered as the cause of the patient's febrile episodes. PSH is a common but unrecognized complication after TBI and is characterized by hypertension, tachycardia, sweating, tachypnoea and hyperthermia, the last being less frequent than the other signs[1].
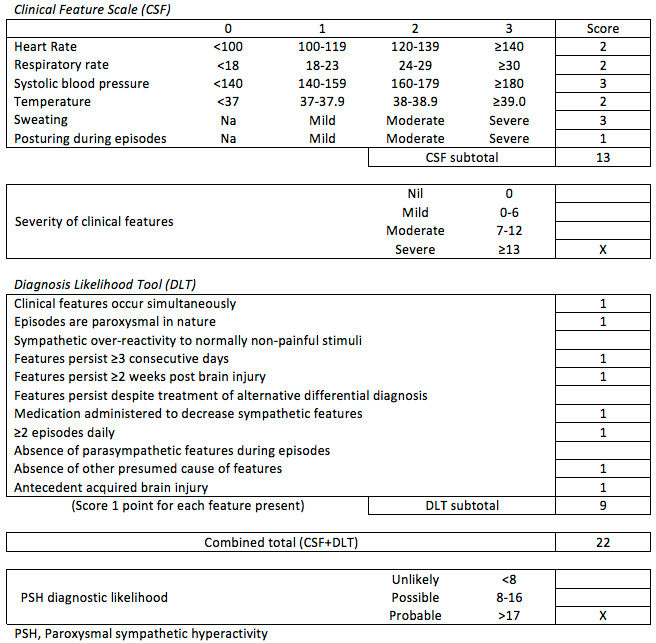
A consensus statement was issued only recently on the definition, nomenclature and diagnostic criteria for PSH, an entity that was previously poorly recognized, thus leading to delays in treatment and increased morbidity among TBI patients. In this consensus, an assessment measure was proposed combining a "Clinical Feature Scale" and a "Diagnosis Likelihood Tool"[2]. Our patient scored 22 points in this proposed model, indicating a 'Probable' PSH diagnosis (Table 1).
Current state-of-the art treatment for this condition with beta-blockers was initiated with propranolol 10 mg every 8 hours up-titrated to 30 mg every 6 hours on discharge[3]. The patient experienced complete resolution of all the described symptoms and no negative beta-blocker side-effects were noticed.
DISCUSSION
PSH has only been defined recently[2]. Previously, the lack of a definition and diagnostic criteria resulted in a poorly understood condition with a variety of symptoms that made recognition difficult. Although it has been known about for more than 60 years, it had over 31 different eponyms, making it very difficult to identify[2,4].
Recognition of this syndrome is crucial for faster recovery in TBI patients, even while still in intensive care units, thus reducing complication rates and length of stay[5].
This is a common syndrome and failure to recognize it is associated with increased morbidity and mortality, higher health costs, longer hospitalizations and poorer outcomes[2]. This case report highlights the implications of missing this diagnosis as the patient had previously been denied admittance to a rehabilitation hospital.