ABSTRACT
Sinus histiocytosis with massive lymphadenopathy (SHML) is a rare and benign cause of lymphadenopathy and was first described in 1969. This disease commonly presents in children and young adults with supra-diaphragmatic lymphadenopathy mainly at cervical nodal sites, composed of a population of histiocytes. Since its description, over 400 cases have been described, but there are few reports in the literature on its association with lymphomas. This case report describes a case with co-existing SHML and anaplastic large cell lymphoma (ALCL). The diagnosis of SHML in our patient did not alter the clinical outcome and the patient responded well to treatment for ALCL. Clinicians should maintain a high index of suspicion in cases of infra-diaphragmatic SHML for the presence of occult lymphoma.
LEARNING POINTS
- A rare presentation of sinus histiocytosis with massive lymphadenopathy (SHML) with anaplastic large cell lymphoma in the same lymph node at the same time is described.
- SHML has no proven clinical significance./li>
- A diagnosis of SHML in the presence of infra-diaphragmatic lymphadenopathy should raise a high index of suspicion for lymphoma.
KEYWORDS
Sinus histiocytosis with massive lymphadenopathy; Rosai Dorfman disease; anaplastic large cell lymphoma; immunohistochemistry
INTRODUCTION
A rare association of infra-diaphragmatic sinus histiocytosis with massive lymphadenopathy (SHML) (Rosai-Dorfman disease) and anaplastic large cell lymphoma (ALCL) in the same lymph node is described.
CASE REPORT
A 16-year-old boy was admitted to the surgery department with a 6-month history of insidious onset of gradually progressive dragging upper abdominal pain and significant weight loss. Clinical examination was remarkable for pallor, hepato-splenomegaly and a firm epigastric mass. However, there was no significant palpable lymphadenopathy. Laboratory investigations showed moderate anaemia with raised ESR and LDH levels. Serology and other laboratory tests were negative. Abdominal ultrasonography revealed moderate grade hepato-splenomegaly with multiple lymph nodes in mesenteric, omental, peri-pancreatic, peri-splenic, para-caval and para-aortic locations. The large retro-peritoneal nodal masses encased coeliac vessels.
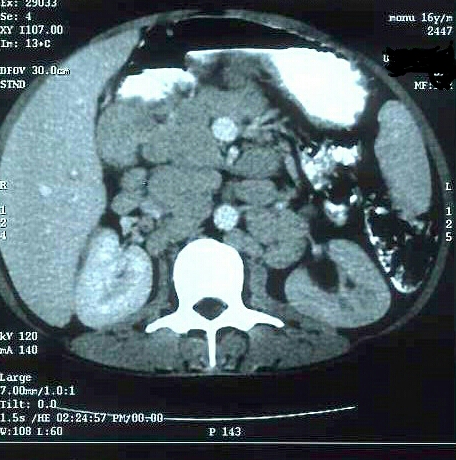
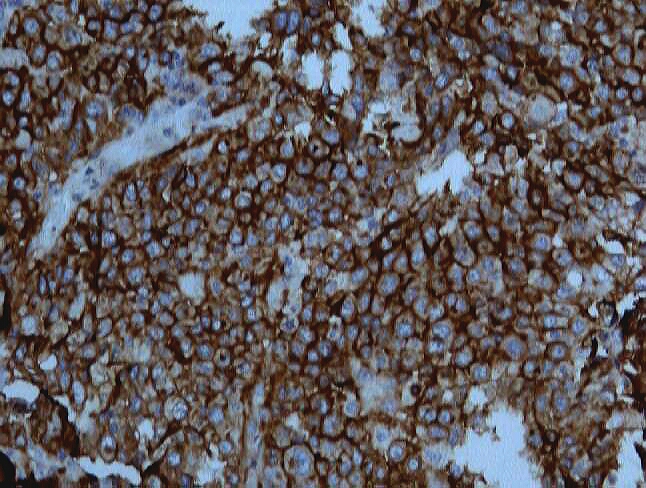
These findings were confirmed by contrast enhanced computed tomography and were suggestive of lymphoma (Fig. 1). There was no significant supra-diaphragmatic lymphadenopathy. The patient underwent retro-peritoneal lymph node biopsy and specimens were subjected to histopathological examination (HPE) which revealed markedly dilated sinuses filled with numerous histiocytes having abundant pale cytoplasm, round to oval nuclei, a single nucleolus and evidence of lympho-phagocytosis (emperiolysis). These cells showed strong focal CD68 and S-100 expression, but CD1a, cytokeratin and HMB-45 markers were negative thus excluding Langerhan's cell histiocytosis, epithelial pathologies and melanoma, respectively. The findings were strongly suggestive of sinus histiocytosis and hence the patient was referred to the department of medicine. In view of his clinical deterioration, we decided to perform ultrasound-guided fine needle aspiration cytology of mesenteric lymph nodes. Microscopic examination of these nodes showed atypical lymphoid cells showing marked pleomorphism, eccentric irregular nuclei, reticulo-glandular nuclear chromatin, prominent nucleoli and abundant cytoplasm. Giant cell forms were also seen, suggestive of large cell lymphoma. The retroperitoneal lymph node biopsy sections were therefore subjected to HPE a second time. Anaplastic large cells were seen in cohesive clusters in sinuses, para-cortex and sub-capsular areas which strongly expressed CD30 and epithelial membrane antigen (EMA) (Fig. 2). In view of the positive ALK antigen, negative T and B cell markers and no extra-nodal involvement, a final diagnosis of ALK-positive primary systemic anaplastic large cell lymphoma, 'null cell' type was made.
Figure 1. CT abdomen showing lymphadenopathy
Figure 2. CD30 antigen positive tumour cells of anaplastic large cell lymphoma (ALCL) in a retro-peritoneal lymph node section
DISCUSSION
What is already known
HML, also known as Rosai-Dorfman disease (RDD), was first described by Rosai and Dorfman in 1969 as a distinct clinico-pathological entity. It is a rare non-neoplastic, usually self-limiting disease of unknown aetiology. It most commonly presents as a bilateral painless cervical lymphadenopathy in a young individual with spontaneous resolution but infrequently may remain indolent for years. There is a pathological increase in the number of histiocytes, mainly mononuclear phagocytic cells and antigen-presenting cells of bone marrow origin. This entity has a unique histopathological appearance that distinguishes it from other processes. This is supported by findings which are strongly positive for S-100 protein but negative for CD1a marker[1].
ALCL, also called Ki-1 lymphoma, is a morphological and immunological distinct subset of non-Hodgkin lymphoma, originally described by Stein et al. in 1985. It accounts for 2–8% of all lymphomas with a male to female ratio of 6.5:1. It is characterized by proliferation of pleomorphic large neoplastic lymphoid cells which strongly express CD30 antigen (Ki-1 antigen), usually growing in a cohesive pattern and preferentially spreading in the lymph node sinuses. Primary systemic ALCL generally has an aggressive clinical course with frequent systemic and extra-nodal spread, although response to treatment and overall survival is good in ALK-positive younger patients[2].
The association of SHML with lymphoma is rare and very few cases have been reported in the literature[3]. There is temporal dissociation between SHML and lymphoma in the majority of reviewed cases with only very few having concurrent presentation[4]. However, both entities occurred in same lymph node concomitantly in our case. Interestingly, predominantly retro-peritoneal nodal sites rather than cervical sites have been reported in the majority of cases. Similar involvement was seen in our case as well. Foci of SHML were identified in retro-peritoneal lymph nodes within sinuses and in between neoplastic ALCL nodules involving less than 20% of total lymph node tissue examined histologically.
What is new
The aetiopathogenesis of SHML in the setting of lymphoma is unknown, although some studies suggest a role for EBV and HHV-6 whereby lymphoma-induced immunodeficiency predisposes the individual to these infections. Another possibility is that SHML is a response to underlying immune dysregulation associated with malignant lymphoma[4]
Why it is significant
The presence of SHML in our patient was an incidental finding and had no clinical significance as the patient achieved complete clinical remission following treatment of ALCL with standard chemotherapy. Although simultaneous SHML and ALCL is very rare, a diagnosis of concomitant malignant lymphoma should be considered especially if the clinical course is atypical for SHML[5].