ABSTRACT
Objective: To describe hypocalcaemia due to vitamin D deficiency in 'hikikomori' syndrome.
Materials and methods: A 37-year-old man with 'hikikomori' syndrome for a year was admitted with hypocalcaemia (serum ionic calcium 1.17 mmol/l). Serum 1,25(OH)2-vitamin D3 determined by liquid chromatography–tandem mass spectrometry was depressed at 12.1 pg/ml (29.0 pmol/l) and plasma intact PTH elevated at 324 ng/l. Administration of 1 μg/day 1α(OH)-vitamin D3 and 1 g/day calcium lactate for 1 week normalized calcium and PTH, and raised 1,25(OH)2-vitamin D3 to low normal levels.
Conclusion: This is the first report of hypocalcaemia due to vitamin D deficiency in a patient with 'hikikomori' syndrome.
LEARNING POINTS
- A patient with psychiatric disorders can develop endocrine/metabolic abnormality.
- Hikikomori syndrome should be listed as a possible cause of hypocalcaemia in adults.
- Early diagnosis of hypocalcaemia in hikikomori syndrome prevents bone damage.
KEYWORDS
Hikikomori syndrome, Hypocalcaemia, Hypovitaminosis D
CASE DESCRIPTION
'Hikikomori' syndrome has been described as complete withdrawal from society for 6 months or longer[1]. In the English version of Oxford Dictionaries, hikikomori is defined as (in Japan) the abnormal avoidance of social contact, typically by adolescent males. A person who avoids social contact. Origin: Japanese. literally "staying indoors, (social) withdrawal". There are almost 1 million hikikomori in Japan between the ages of 20 and 40. Hikikomori syndrome[1,2] is regarded as a mental or psychiatric disorder and most probably for this reason, metabolic abnormality, in particular hypocalcaemia, associated with this condition has not been described.
A 37-year-old man was admitted due to hypothermia and bizarre behaviour in mid-winter. He was found by his family unresponsive to verbal stimuli with rectal incontinence in his room without clothing or heating: the room temperature was 10°C. He had lived with his parents for about a year but rarely left his room, except for an occasional short walk at night. His past and family history was otherwise unremarkable except for his mother's hypertension.
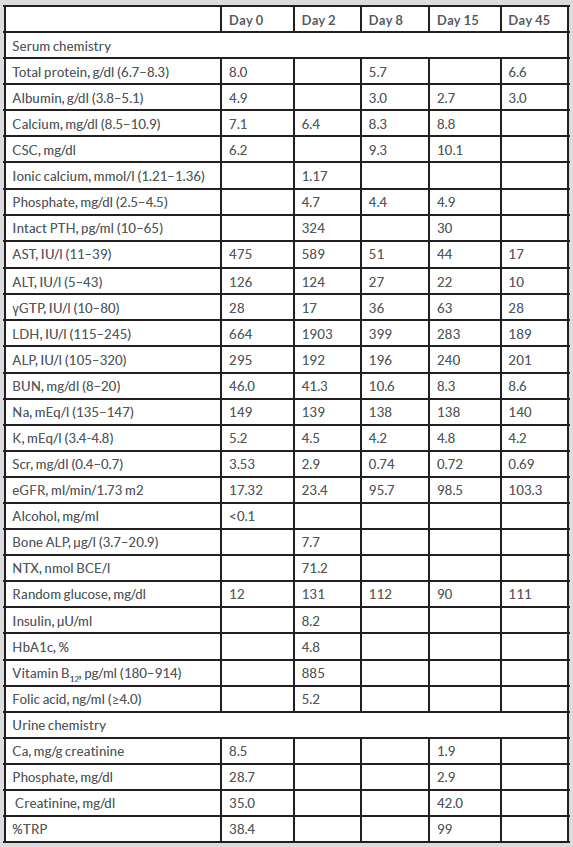
Upon admission, his rectal temperature was 30.9°C, consciousness was Glasgow Coma Scale 3 (E1V1M1), blood pressure was 84/46 mmHg and pulse rate was 72/min, regular. His BMI was 20.5 kg/m2. There was generalized muscle weakness but Chvostek's and Trousseau's signs were negative. The patient had hypocalcaemia, as shown by an albumin-corrected serum calcium concentration (CSC) of 1.6 mmol/l, ionic calcium of 1.17 mmol/l (reference range, 1.21–1.36) and low urinary excretion of calcium of 0.009 mg/g creatinine (Table 1). ECG showed normal sinus rhythm and QTc was within the normal range at 0.416 sec. He also had hypoglycaemia, hypernatraemia and hyperkalaemia. Serum levels of hepatic enzymes except for γGTP were elevated; the serum alcohol concentration was not elevated. Renal function was also impaired (Table 1). Serum levels of vitamin B12 and folic acid were normal. Treatment with fluid and external warming was instituted, and the patient's body temperature rose to 36.5°C within 6 hours and consciousness was normalized by day 2. Hypocalcaemia was investigated further.
Table 1. General laboratory data
ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BCE/l, nmol bone collagen equivalents/l; BUN, blood urea nitrogen; CSC, albumin-corrected serum calcium; γGTP, gamma-glutamyl transpeptidase; eGFR, estimated glomerular filtration rate; LDH, lactate dehydrogenase; NTX, collagen type 1 cross-linked N-telopeptide; PTH, parathyroid hormone; Scr, serum creatinine; %TRP, percent tubular reabsorption of phosphate.
Medications are described in the footnote of Table 2.
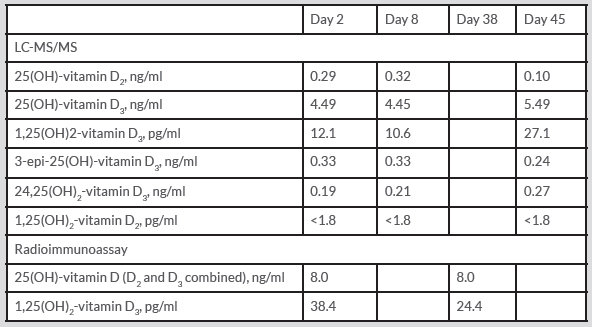
Initially, determination of 25(OH)-vitamin D (D2 and D3 combined) (Diasorin, Stillwater, MN), 1,25(OH)2-vitamin D3 (Immunodiagnostic Systems, Gaithersburg, MD) by radioimmunoassay (RIA) and intact parathyroid hormone (PTH) by electrochemiluminescence assay (Elecsys, Roche, Basel, Switzerland) was carried out at Special Reference Laboratories, Tokyo. Upon receiving an unexpectedly normal value for 1,25(OH)2-vitamin D3 (Table 2), serum levels of vitamin D and related molecules were re-determined by liquid chromatography–tandem mass spectrometry (LC-MS/MS)[3–5].
Serum concentrations of vitamin D and its precursors and metabolites are shown in Table 2. LC-MS/MS indicated that levels of vitamin D and its precursors and metabolites were all depressed, particularly 1,25(OH)2-vitamin D3. It should be noted that the values obtained by RIA for 25(OH)-vitamin D (D2 and D3 combined) and 1,25(OH)2-vitamin D3 were within the reference range. The plasma level of intact PTH was markedly elevated and urinary excretion of phosphate was elevated as indicated by low tubular reabsorption of phosphate. Bone alkaline phosphatase and collagen type 1 cross-linked N-telopeptide (NTX) were within the reference range (Table 2).
Table 2. Serum levels of vitamin D and related substances before and after treatment
LC-MS/MS, liquid chromatography-tandem mass spectrometry.
Medications were as follows. 1α(OH)-Vitamin D3: 1 μg/day from day 2 to day 15, 0.5 μg/day from day 16 to day 17, withdrawn from day 18 to day 41, 0.25 μg/day from day 42, and on. Calcium lactate: 1 g/day from day 2 to day 10, withdrawn from day 11 to day 34, 1 g/day from day 35, and so on. Calcium carbonate: 1 g/day from day 11 to day 34.
Hypocalcaemia was diagnosed as caused by vitamin D deficiency arising from insufficient ultraviolet B irradiation due to hikikomori syndrome. Oral administration of 1 μg/day 1α(OH)-vitamin D3 and 1 g/day calcium lactate was begun. Treatment raised serum calcium levels within a week and normalized plasma intact PTH within 15 days (Table 2). At the same time, generalized muscle weakness disappeared. The plasma 1,25(OH)2-vitamin D3 level remained low at this stage but rose to the low normal range by day 45.
DISCUSSION
Vitamin D deficiency in adults is not uncommon and frequently due to inadequate exposure to sunlight. Because of prolonged social withdrawal, patients with hikikomori syndrome may develop vitamin D deficiency due to inadequate exposure to sunlight. Nonetheless, hypocalcaemia and/or vitamin D deficiency has not previously been reported in hikikomori syndrome[1,2] and may have been overlooked. In fact, Chvostek's and/or Trousseau's signs were both negative in this case, and hypocalcaemia was found incidentally during the general laboratory investigation. The lifestyle of this patient was typical of 'hikikomori' syndrome in that he had no exposure to sunlight for about a year. Consequently, the pathophysiology of this patient was similar to rickets. Nonetheless, bone alkaline phosphatase and NTX were normal, indicating that bone turnover had not yet been depressed.
Importantly, the RIA method commonly used to assess vitamin D and related molecules may not be reliable when levels are very low, as in this patient, since RIA overestimated vitamin D and a precursor molecule, as reported elsewhere. Therefore, RIA should not be relied on solely to diagnose vitamin D deficiency, with LC-MS/MS being a better choice[3–5].
In conclusion, we have described hypocalcaemia in 'hikikomori' syndrome arising vitamin D deficiency for the first time. Further studies are warranted to establish the prevalence and severity of hypocalcaemia and vitamin D deficiency in this syndrome. LC-MS/MS instead of RIA is recommended as the method to determine levels of vitamin D and its metabolites in order to assess vitamin D levels.