ABSTRACT
Platypnoea-orthodexia syndrome is a rare cause of dyspnoea when hypoxaemia is induced by the upright position and relieved by recumbency. We report two cases in which platypnoea-orthodexia syndrome was present and caused by two different mechanisms: intracardiac shunt and intrapulmonary shunt.
LEARNING POINTS
- Platypnoea-orthodexia syndrome should be considered in the differential diagnosis of unexplained hypoxia.
- A high degree of suspicion is required to instigate initial investigations with either postural pulse oximetry or arterial gas analysis.
- The diagnosis must be based on the presence of both an anatomical and a functional component.
KEYWORDS
Platypnoea-orthodexia, hypoxia, shunt
CASE HISTORY 1
An 81-year-old woman with hypothyroidism was referred to the emergency department with a 3–4-month decline in exercise tolerance, dizziness and difficulty with word finding, which had worsened over the previous 5 days.
There was no history of syncope, focal weakness or slurred speech. The patient was afebrile with no complaint of infective symptoms. She had never smoked or had exposure to industrial dusts or asbestos. Daily medications were ramipril 10 mg, aspirin 75 mg and levothyroxine 50 µg. On arrival, the patient was hypertensive (192/104 mmHg), tachycardic (100 bpm) and hypoxic with oxygen saturations of 86% in room air. Heart sounds were normal, chest was clear, and the abdomen and neurological examination were normal.
Admission blood analysis showed elevated C-reactive protein (CRP) at 112 mg/l, white blood cells 3.6×109/l, and normal urea, electrolytes and liver function tests. An electrocardiogram demonstrated sinus tachycardia. Chest x-ray and brain imaging were normal. Oral antibiotics were started because of the elevated CRP.
In view of the patient's hypoxia, a CT pulmonary angiogram (CTPA) was organized, revealing background chronic pulmonary disease with no evidence of fibrosis, pulmonary emboli or consolidation. Pulmonary function tests found normal lung volumes with no evidence of airflow obstruction and normal gas transfer.
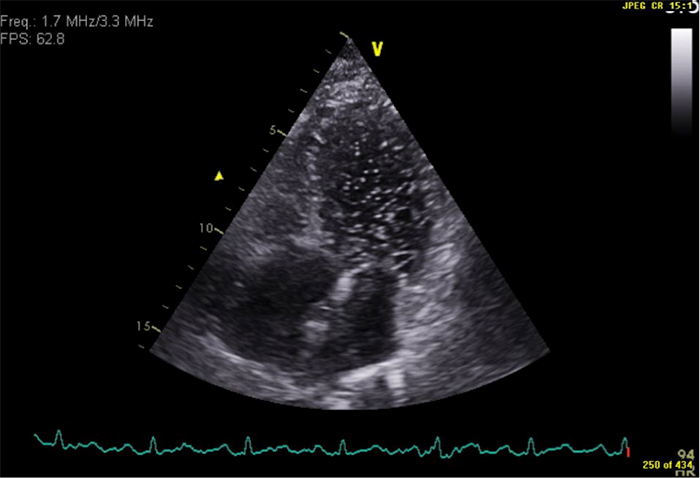
Arterial oxygen partial pressure in air when recumbent was 8.86 kPa compared with 6.62 kPa when upright. Transthoracic microbubble contrast echocardiography revealed a large intracardiac shunt, good biventricular function and no significant valve defect (Fig. 1). Cardiology personnel planned for transoesophageal echocardiography on a tilt table but the patient declined further investigation. Her oxygenation improved slowly over 1 week and she was discharged.
CASE HISTORY 2
A 27-year-old woman with endometriosis and polycystic ovarian syndrome and previous positive pressure ventilation for acute respiratory distress syndrome in the context of urosepsis, presented to the emergency department acutely breathless. Her general practitioner had prescribed a course of oral antibiotics, which had not improved her symptoms. She had a cough, productive of green sputum, described rigors and mentioned having diarrhoea during the preceding 2 weeks, which had since resolved. She had never smoked and was not taking any regular medication.
On admission, her chest radiograph and inflammatory markers were normal. Despite routine intervention for community-acquired pneumonia, she deteriorated clinically and became more dyspnoeic and tachypnoeic (36 bpm). Pulse oximetry with an inspired oxygen fraction of 0.6 was 97% when lying, and 84% when upright. Heart rate was 93 bpm, blood pressure was 107/76 mmHg, and chest was resonant, with crepitations in the right base and widespread rhonchi. The patient was admitted to our high dependency area for observation and improved without the need for respiratory support. Microbubble contrast echocardiography showed good systolic function, no valve abnormality and no intracardiac shunt. Viral titres for influenza type A were slightly elevated, with remaining viral serology being normal. Pulmonary function tests 2 weeks after discharge were normal.
PLATYPNOEA-ORTHODEOXIA
Provokeable hypoxaemia when in the upright position led to the diagnoses of platypnoea-orthodeoxia in our two patients. This is a well-described, yet rarely considered syndrome, where dyspnoea and arterial hypoxaemia is associated with assumption of the upright posture and relieved by recumbence. It was first described in 1949 by Burchell[1] and later named in 1969[2].
It is dependent on the coexistence of an anatomical and a functional component and has been associated with cardiac, pulmonary and hepatic disease, but the mechanism is different in each situation.
First, there must be an anatomical communication between the left and right circulation which is most frequently intracardiac, in the form of a patent foramen ovale[3], although intrapulmonary communication has been described[4]. This communication must have the potential to shunt deoxygenated blood from the right circulation to the well-oxygenated left circulation, which is unusual as a shunt is expected to be left-to-right due to relative, physiological, increased left cardiac pressures.
Second, this right-to-left shunt must develop, or be worsened, by assumption of an upright posture and resolve when recumbent[5]. It is this functional, positional component that distinguishes this syndrome from other cyanotic heart conditions where there is a persistent right-to-left shunt, as in Eisenmenger's syndrome.
Postural right-to-left shunt is triggered by anatomical abnormalities, for example, directing blood flow from the vena cava directly towards an atrial defect and into the left atrium[6] as may occur with a prominent Eustachian valve[7], elongated/tortuous aortic root, papillary rupture or atrial septal aneurysm, many of which are more frequently seen in the elderly[5] or following surgery for lung resection, thoracic trauma or previous TB[6].
Functional intrapulmonary shunt can arise as a result of changes in alveolar perfusion gradients. In the normal lung, blood flow is greatest, due to gravity, in the bases compared to the apices. It is proposed that when alveolar pressure is increased due to lung disease and altered ventilatory mechanics, an upright posture may increase this tendency of greater blood flow in the bases, because of a drop in pulmonary artery pressure leading to compression of pulmonary capillaries by alveoli, resulting in increased dead space, thus instigating a vicious cycle of dyspnoea, hyperventilation and air-trapping. Failure of the sympathetic vasoconstrictor response to hypoxaemia may contribute to this effect[8]. For similar reasons, it has been postulated that symptoms may worsen with dehydration[4] and have also been reported in acute respiratory distress syndrome[9].
Treatment
Treatment is of the precipitating cause. Where this is intracardiac, closure of the shunt in many cases prompts a dramatic reduction in symptoms. Prone ventilation in cases of acute respiratory distress syndrome has reduced right-to-left shunt with corresponding improvement in arterial gasses[10]. Volume replacement is required if the patient is dehydrated and infection should be treated with antibiotics. Where hepatopulmonary syndrome is the cause, resolution is more difficult with these patients often requiring a liver transplant[4].
CONCLUSION
Platypnoea-orthodeoxia is a diagnosis easily missed without a high degree of suspicion. It can be investigated non-invasively with peripheral pulse oximetry or arterial blood gas analysis in the upright and supine position. If orthodeoxia is demonstrated, transthoracic echocardiography with microbubble contrast should be performed to determine if an intracardiac shunt is present. This is a non-invasive test with an excellent safety profile when compared to cardiac catheterisation. Sensitivity is increased if contrast is injected via the leg as the majority of shunts occur at the level of the inferior vena cava. Sensitivity is also increased when positive end-expiratory pressure is increased by coughing or the Valsalva manoeuvre[6].