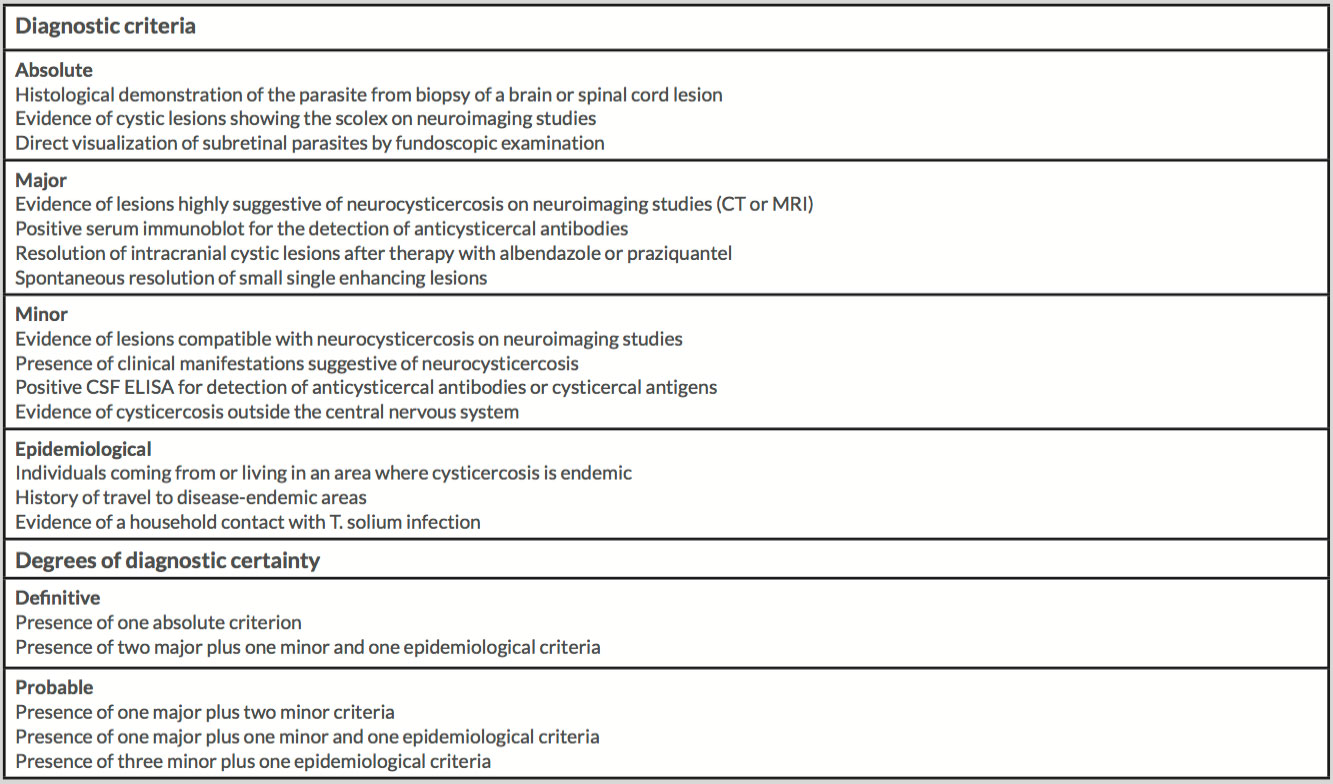
ABSTRACT
Cysticercosis is triggered by infection with the larval form of the tapeworm Taenia solium. The usual sites for the development of cyscticerci are the central nervous system (neurocysticercosis – NCC), subcutaneous tissue, skeletal muscle, heart muscle, and the eye. Ocular cysticercosis is caused by the growth of the larvae within ocular tissues. The extraocular muscles form is the most common type of orbital cysticercosis. We report a case of a patient admitted with seizures secondary to NCC, who developed ocular symptoms after starting combined treatment with albendazole, praziquantel and dexamethasone. The investigation revealed a cystic lesion in the lateral rectus muscle.
LEARNING POINTS
- Neurocysticercosis (NCC) is the main cause of epilepsy in someone coming from an endemic area; therefore, it is imperative to have a high index of suspicion.
- Ocular cysticercosis can present at the time of diagnosis or can be triggered by the cysticidal treatment.
- Before starting cysticidal treatment, systemic corticosteroid should be used in order to reduce the inflammatory response secondary to the release of toxins following the death of the parasite.
KEYWORDS
Neurocysticercosis (NCC), Taenia solium, orbit, extraocular muscles, dexamethasone
CASE DESCRIPTION
We present a 38-year-old male from Cape Verde, resident in Portugal. His last trip to Cape Verde had been two years previously. He has a history of alcohol and tobacco dependence. Six years previously, he had been admitted to the emergency department after collapsing.
A cranial computed tomography (CT) scan revealed multiple punctiform calcifications in both cerebral hemispheres and in the cerebellum, surrounded by a small cyst and with an eccentric position, suggestive of parasitic infestation - cysticercosis. On the infectious diseases ward, treatment began with albendazole and dexamethasone. Beyond cysticidal treatment for NCC, carbamazepine was started as the diagnosis of secondary epilepsy was established.
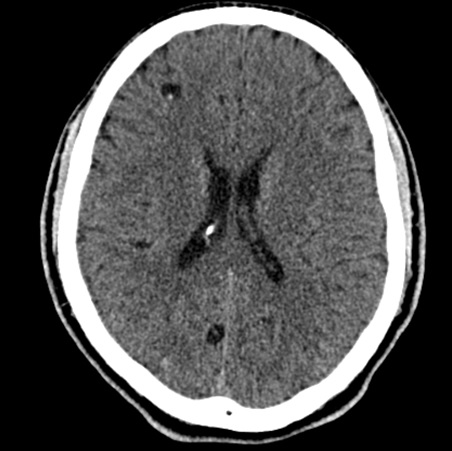
In April 2016, he was admitted again to the Emergency Department after a convulsion, presenting without fever or other neurological symptoms. He had undergone a cranial CT scan (Figs. 1 and 2) that showed similar findings to those found 6 years earlier. Laboratory results: Hb 136 g/L, WBC 6.57 10×9/L, Neutrophils 82%, Eosinophils 0.3%, Platelets 228 10×9/L, C-Reactive Protein 3 mg/L, Aspartate Phosphatase 96 IU/L, Alkaline Phosphatase 63 IU/L, Bilirubin 17.1 µmol/L, Carbamazepine level <0.5 mg/L. He was admitted to the infectious diseases ward due to seizures related to NCC, non-compliance to carbamazepine, and alcohol dependence.
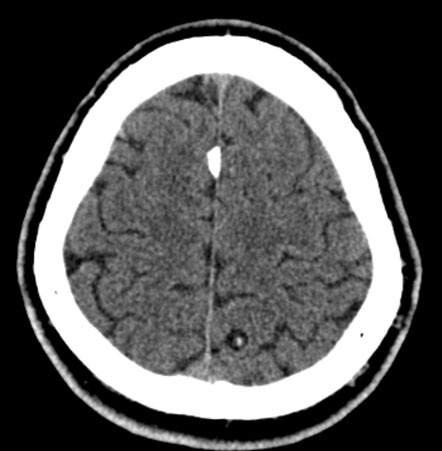
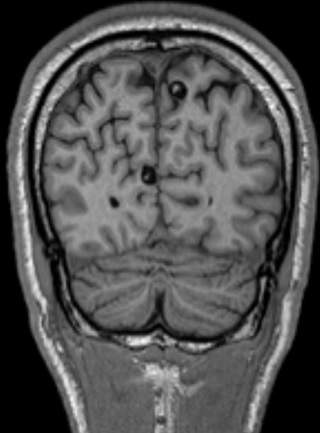
He was treated with dexamethasone 10 mg 8/8h, carbamazepine, albendazole and, 4 days later, praziquantel. He was observed by the ophthalmology department, which documented right conjunctival hyperaemia and normal fundoscopy. An EEG showed slightly slow base activity without epileptic activity. An MRI was also performed (Fig. 3) and confirmed the CT scan results. After 8 days of albendazole and dexamethasone (and 4 days of praziquantel), he presented with sudden onset of left eyelid oedema and left ocular pain that increased with horizontal eye movements. An orbital CT scan revealed thickening and densification of the left lateral rectus muscle (Fig. 4), with an apparent cystic lesion with hypodense centre, suggestive of infiltration by cysticercosis. Analgesia was started, and the dexamethasone dose was increased from 10 mg 8/8h to 10 mg 6/6h, with significant clinical improvement. The patient was discharged and the outcome was favourable. At re-evaluation, he continued taking carbamazepine, and confirmed no recurrence of seizures or ocular symptoms.
Figure 1. CT scan showing two cystic lesions in both cerebral hemispheres
Figure 2. CT scan showing one cystic lesion on the left hemisphere
Figure 3. MRI showing two cystic lesions in both cerebral hemisphere
Figure 4. CT axial showing thickening of the left lateral rectus muscle
DISCUSSION
We decided to report this clinical case because cysticercosis remains a challenge for European care providers[1]. As the larvae display a strong affinity for the central nervous system[2], NCC is the most common helminthic neurological infection and a major public health problem in most of the world[3]. In Portugal, as in the rest of Europe, autochthonous cases are disappearing, while imported cases are rising as a consequence of travel and migration[1]; most of the cases are imported from immigrants from Portuguese colonies, such as Cape Verde, Angola, Mozambique, Guinea-Bissau and São Tomé and Príncipe[1].
NCC is the most common cause of acquired epilepsy worldwide, being the main cause of epilepsy in someone coming from an endemic area[1]. Millions of individuals are estimated to be infected, many of whom become symptomatic at some point in their lives[3]. The parasite load, dependent on both the size and number of cysticerci, is an important determinant of symptomatology[2]. NCC may remain asymptomatic for months to years and sometimes its diagnosis is made incidentally when neuroimage is performed[4]. Diagnosis is based on neuroimaging (cystic lesions showing the scolex on CT or MRI) and confirmed by serology[3]. Accurate diagnosis is possible after interpretation of clinical data with findings of neuroimaging studies and immunological tests[5]. Del Brutto et al. proposed a set of diagnostic criteria that combine aspects of clinical history, neuroimaging and immunological evidence, as well as epidemiological factors, to form defined guidelines for the diagnosis of NCC[6] (Table 1).
Our patient had a background of previous NCC and had been to Cape Verde two years previously.
Ocular cysticercosis may be extraocular (in the subconjunctival or orbit tissues) or intraocular (in the vitreous, subretinal space, or anterior chamber)[4]. Ocular manifestations of cysticercosis vary from asymptomatic to a painful blind eye and may be associated with neurological symptoms such as headaches, fits, diplopia, restriction of ocular movements, and visual problems[4]. One of the first symptoms of extraocular cysticercosis is double vision (diplopia) from misalignment of the visual axes[4]. In our patient, the symptoms started 8 days after beginning treatment. Symptom exacerbation is common during the first week after antiparasitic treatment is initiated. The use of steroids is important at this point in order to decrease the effect of the strong inflammatory response, secondary to the release of toxins following the death of the parasite.
Authors suggest that steroids should be administered for around 3 days before the cysticidal drugs are started, then continued for approximately 1 week following the end of the course[2]. In our patient, it is likely that the dose of steroids was probably not sufficient. The two most widely accepted cysticidal drugs are albendazole and praziquantel. These drugs are only applicable in the treatment of viable cysts in the vesicular or early colloidal stages of development, and are ineffective against calcified cysts. The combination of albendazole and praziquantel increases the parasiticidal effect in patients with multiple brain cysticercosis[3]. Therapeutic approaches might include symptomatic therapy, antiparasitic treatment, or surgery[3]. Medical treatment has no role in the management of intraocular cysticerci due to the potential sight-threatening side-effects of toxin release following the death of the parasite. Surgical treatment is the best choice in intraocular cysticercosis, while medical treatment is the best choice for extraocular presentations including extraocular muscles cysticercosis[4].
This is a classic clinical case of NCC, in a patient with non-adherence to antiepileptic drugs and alcoholic habits. However, the ocular symptoms connected to the cyst in the left lateral rectus muscular are unusual.