ABSTRACT
Bartter syndrome is a rare heterogeneous disease characterised by a deficiency in sodium and chloride absorption. Gain-of-function mutations in the CASR gene have been described in some patients with Bartter syndrome associated with hypocalcaemia and hypercalciuria. We describe a case of adult-onset Bartter syndrome with hypocalcaemia severe enough to cause osteomalacia.
LEARNING POINTS
- Bartter syndrome is one of the rare heterogenous diseases that present with electrolyte disturbances.
- Bartter syndrome type 5 also causes hypercalciuria which is not severe enough to cause osteomalacia.
- Patients with adult-onset Bartter syndrome should be screened promptly for osteomalacia to prevent pathological fractures and consequent complications.
KEYWORDS
Bartter syndrome, metabolic alkalosis, hypokalemia, hypocalcemia, osteomalacia, CaSR
INTRODUCTION
Bartter syndrome, first described by Bartter in 1962, comprises a set of autosomal recessive renal tubular disorders characterized by hypokalaemia, hypochloraemia, metabolic alkalosis and hyper-reninaemia with normal blood pressure[1]. Symptoms and severity vary between individuals but affected individuals generally have a mild form of the condition. It usually presents in young adulthood and is characterized by polyuria, fatigue, muscle cramps, spasms and tetany. Individuals may have low levels of parathyroid hormone, seizures and paraesthesias[2]. The calcium sensing receptor (CaSR) plays an important role in calcium homeostasis. Gain-of-function mutations in the CASR gene have been reported in some patients with Bartter syndrome associated with hypocalcaemia and hypercalciuria. Studies showed that these mutations result in receptor activation that is more severe than other gain-of-function mutations[3]. We describe a case of adult-onset Bartter syndrome with hypocalcaemia severe enough to cause osteomalacia.
CASE REPORT
A 28-year-old woman was admitted to Darul Sehat Hospital with a 3-month history of generalized weakness and fatigue and severe left hip pain for 2 days.
The first episode of generalized physical aches, fatigue and left thigh pain had occurred 5 years previously when she was admitted to a different hospital and on laboratory work-up was found to have hypokalaemia.
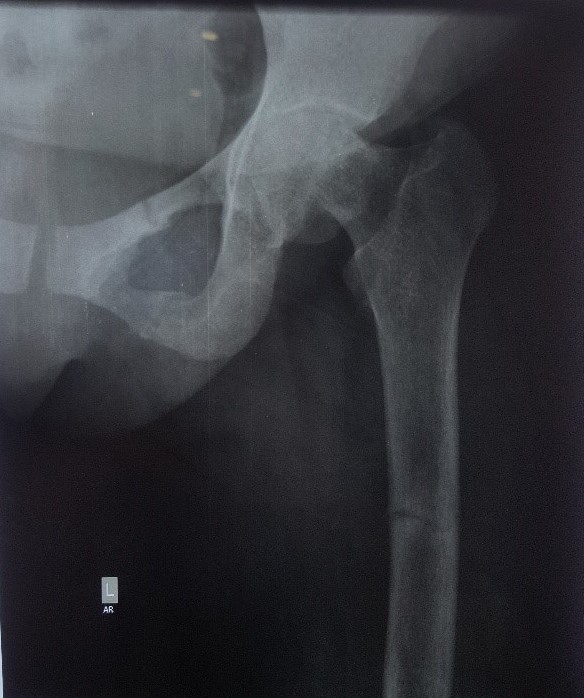
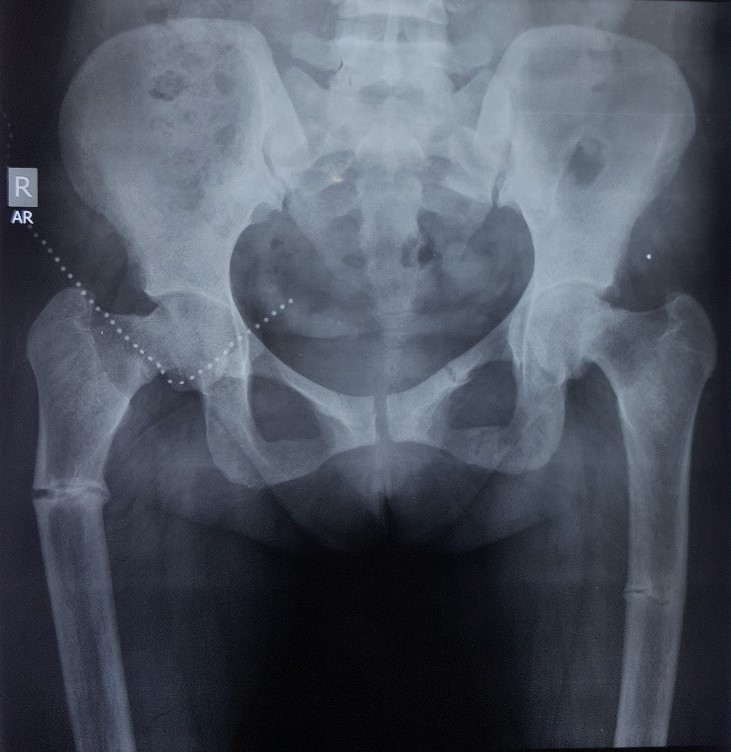
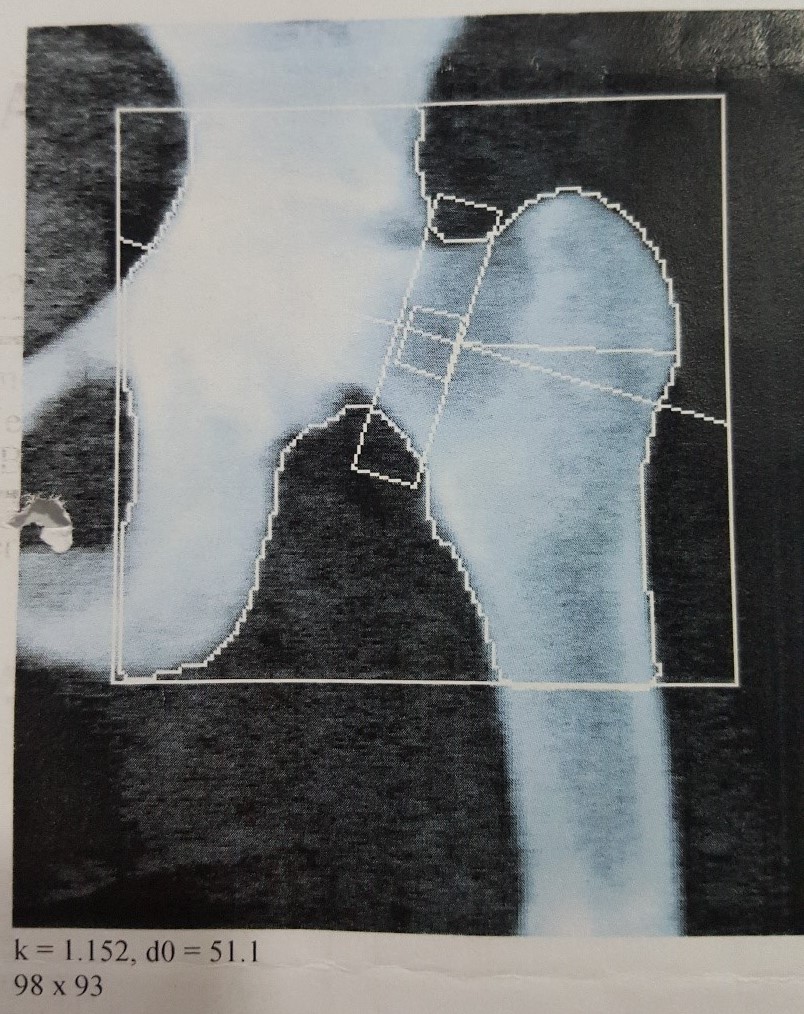
X-rays revealed a fracture of superior ramus of the left pubic bone and proximal parts of the right and left femurs (Figs. 1 and 2). She was conservatively managed for her fractures and her weakness improved with potassium replacement.
Figure 1. X-ray of the left femur and pelvis, February 2012
Figure 2. X-ray of the left femur and pelvis, September 2012
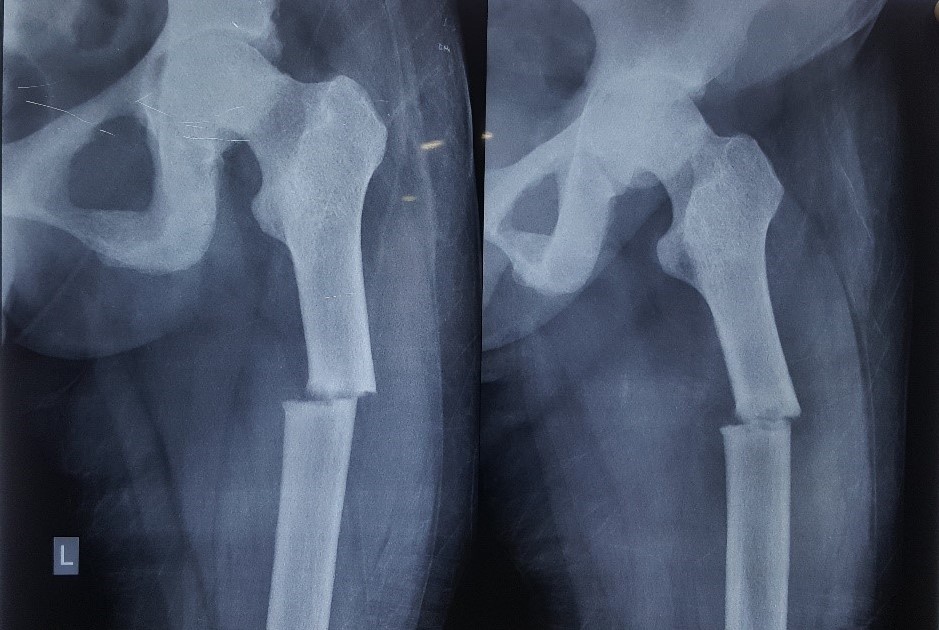
Figure 3. Fracture of the shaft of the left femur, April 2016
Thereafter she had been taking potassium supplements intermittently for her persistent hypokalaemia and calcium supplements but had never been thoroughly investigated. Now she had again developed the same but more severe symptoms. She denied taking laxatives and had no complaints of diarrhoea or vomiting. She had no significant family history and had normal dietary habits.
On examination, the patient appeared relatively well. She was 147 cm tall and a weighed 50 kg. Her pulse rate was 98/min, blood pressure was 100/70 mmHg, and respiration rate was 16/min. Her left thigh was immobile and extremely tender, but there were no open wounds and no loss of sensation or vascular compromise. Examination of all other systems was unremarkable.
Laboratory findings included serum sodium of 136 mEq/l, serum potassium of 2.6 mEq/l, serum chloride of 108 mEq/l, serum bicarbonate of 24 mEq/l, serum calcium of 9.2 mg/dl, serum phosphate of 1.94 mg/dl and alkaline phosphatase of 169 U/l. Blood urea nitrogen was 16 mg/dl, serum creatinine was 0.9 mg/dl and serum magnesium was 2.3 mg/dl.
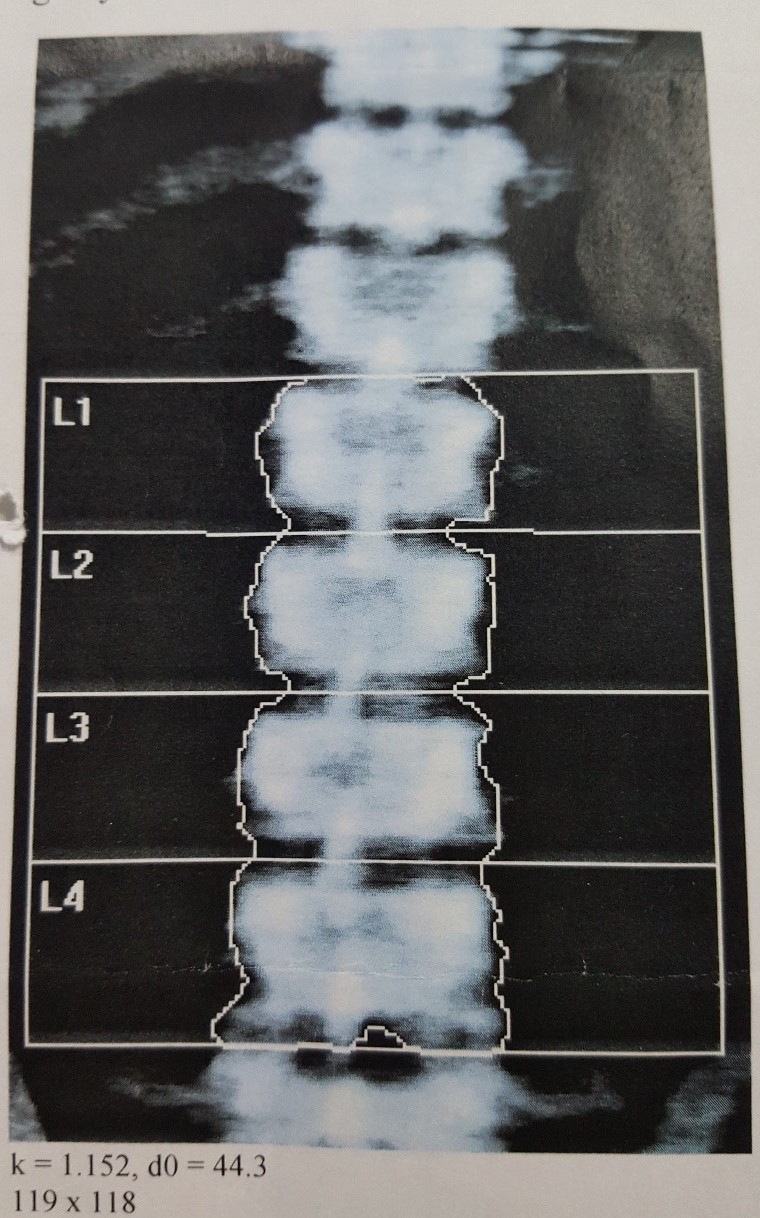
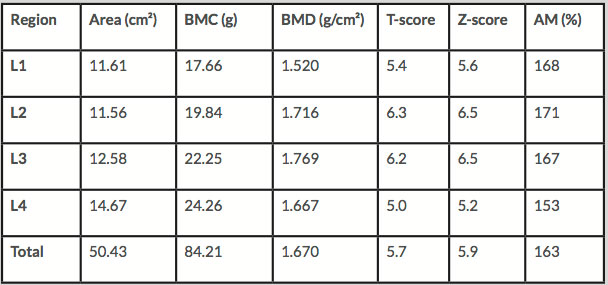
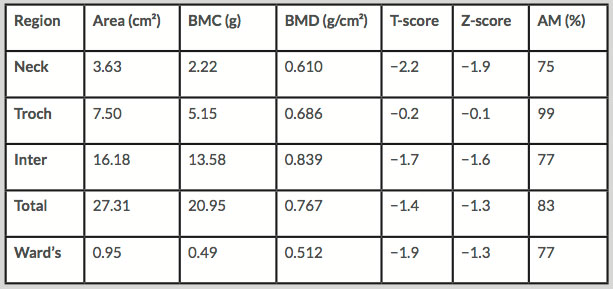
Electrocardiography showed T wave flattening. An x-ray of the left hip joint showed a fracture of the shaft of the left femur (Figs. 1–3). A DXA scan showed osteopaenia with a T-score of −1.9 (Tables 1 and 2, Figs. 4 and 5).
Figure 4. DXA scan, March 2016
Figure 5. DXA scan, March 2016
Table 1. DXA results for the lumbar spine
Table 2. DXA results summary
AM, age matched; BMC, bone mineral content; BMD, bone mineral density.
Serum vitamin D was 31 ng/ml (deficiency: <20 ng/ml). Serum PTH was 182.0 pg/ml (normal: 7–53 pg/ml), plasma renin was 148.0 µIU/ml (normal: 4.4-46.1 µIU/ml erect) and serum aldosterone was 20 ng/dl (normal: <15 ng/ml). The 24-hour urinary excretion of sodium was 182 mEq, potassium 68 mEq, chloride 240 mEq, calcium 120 mg, protein 150 mg and glucose 30 mg, and urine amount was 2,200 ml. The urinary specific gravity was 1.010 and osmolality was 320 mOsm/kg. The patient’s previous laboratory findings when she first started having generalized physical aches and hypokalaemic episodes were serum calcium of 7.62 mg/dl, serum phosphate of 2.48 mg/dl, alkaline phosphatase of 166 U/l and serum potassium of 2.7 mEq/l. The patient was treated with potassium chloride, calcium and vitamin D supplements. Her serum potassium concentration improved from 2.6 mEq/l to 3.1 mEq/l, her muscle strength rapidly recovered and she did well. Her femur fracture was conservatively managed and also began to heal.
DISCUSSION
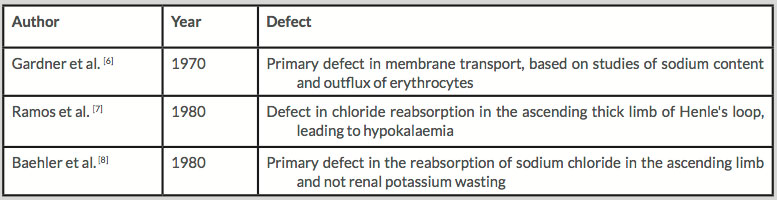
More than 230 different germline mutations of the CaSR, which is encoded by the CASR gene located on chromosome 3q21.1, have been reported. These mutations may cause severe loss of CaSR function associated with hypocalcaemic disorders such as Bartter syndrome type 5, which is characterised by renal salt wasting, hypokalaemic alkalosis and hyper-reninaemic hyperaldosteronism[4].
Four genes have been identified which can cause Bartter syndrome: SLC12A2, encoding the sodium-potassium-chloride cotransporter NKCC2; KCNJ1, encoding the ROMK1 potassium ion channel; CLCNKB, encoding the ClC-Kb basolateral chloride ion channel; and BSND, encoding barttin, a regulatory subunit required for basolateral chloride channel targeting to the membrane. Bartter type 5 is distinguished from the other types by its autosomal dominant transmission and the presence of hypocalcaemic hypercalciuria[5].
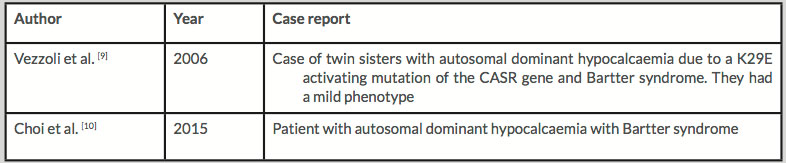
Several studies have described the pathophysiology of this syndrome (Tables 3 and 4). A few cases have been reported, but Bartter syndrome with hypocalcaemia severe enough to cause osteomalacia has not previously been reported.
Table 3. Pathophysiology
Table 4. Case reports
CONCLUSIONS
In this case, the patient was diagnosed with adult-onset Bartter syndrome because of hypokalaemia, relative hypotension, increased renin activity and increased aldosterone level. Following treatment, serum potassium concentration improved and the patient’s muscle strength rapidly recovered. The osteomalacia caused by the disease and found at the same time was also treated and the patient was doing well by her next follow-up visit.