ABSTRACT
We describe a patient with a Salmonella enteritidis mycotic aneurysm. A 91-year-old man presented with recurrent episodes of S. enteritidis bacteraemia 2 months apart. During the second presentation, he underwent magnetic resonance imaging of the left lower limb that revealed rupture of the popliteal artery with a popliteal fossa collection. This was aspirated and cultures grew S. enteritidis. He underwent endovascular stenting and received a prolonged course of antibiotics. Popliteal artery mycotic aneurysm should be considered as a differential in patients presenting with unilateral painful leg swelling and bacteraemia from microorganisms with a propensity for endovascular infections.
LEARNING POINTS
- Our case illustrates a rare and unusual entity of ruptured popliteal mycotic aneurysm in an otherwise common scenario of recurrent nontyphoidal salmonellosis.
- In patients with recurrent Salmonella bacteraemia, clinicians often perform computed tomography scans to look for extraintestinal sites of involvement; however, this frequently misses any peripherally sited aneurysms, which often do not manifest with any early clinical symptoms.
KEYWORDS
Salmonella enteritidis, recurrent salmonellosis, recurrent Salmonella enteritidis bacteraemia, popliteal artery aneurysm
CLINICAL DESCRIPTION
A 91-year-old Chinese man was admitted to our hospital with a 2-week history of progressive left leg swelling and pain associated with intermittent fever. This was a previously healthy patient who had a history of benign prostatic hyperplasia, hypertension, and a previous osteoporotic left intertrochanteric hip fracture.
Two months earlier, he had presented with septic shock secondary to S. enteritidis bacteraemia, sensitive to amoxicillin, trimethoprim/sulfamethoxazole, ceftriaxone and ciprofloxacin. There was no history of gastrointestinal symptoms. Three sets of blood cultures on admission had positive growth. He was screened for human immunodeficiency virus infection, which was negative. Computed tomography (CT) aortogram revealed extensive atherosclerotic calcifications in the aorta but there were no aneurysms or other significant abnormalities. No vegetations were seen on a transthoracic echocardiogram. He was treated with 3 days of intravenous ceftriaxone followed by 4 days of intravenous ampicillin, then discharged from hospital with 7 days of oral ciprofloxacin, for which he was compliant.
On this admission, he was febrile at 38.4°C and tachycardic without hypotension. Clinical examination revealed a swollen left leg that was tender without overlying skin changes.
Methods and procedures
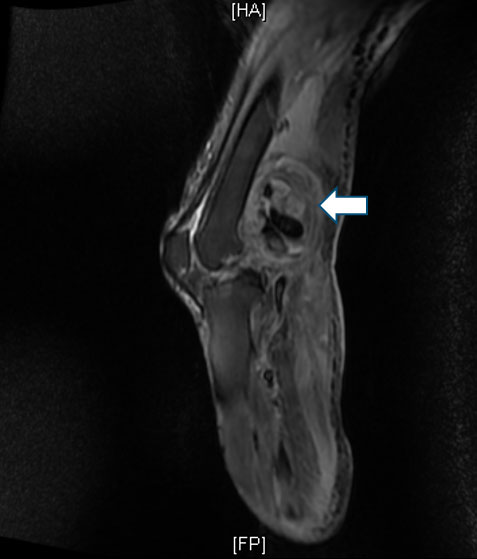
Laboratory evaluation showed a white cell count of 8.7 × 109/L and C-Reactive protein of 279.1 mg/dL. He had biochemical evidence of acute renal impairment and cholestasis on liver function tests. Blood cultures were obtained and these grew S. enteritidis of similar susceptibility to what was isolated 2 months previously. In view of progressive worsening leg swelling and poorly palpated peripheral pulses, magnetic resonance imaging (MRI) of the left leg was performed, with the image as shown in Figure 1.
MRI of the left lower limb revealed a mixed signal intensity lesion in the popliteal fossa consistent with rupture of the popliteal artery. CT angiography confirmed the presence of a collection with gas pockets within the popliteal fossa associated with a leaking popliteal artery pseudoaneurysm.
His popliteal artery was stented and aspiration of the popliteal fossa collection also yielded S. enteritidis, confirming the diagnosis of S. enteritidis ruptured popliteal artery mycotic aneurysm. Repeat blood cultures were negative. He was successfully treated with ciprofloxacin and planned for chronic suppressive therapy in view of the indwelling vascular stent.
Figure 1. Mixed signal intensity collection (white arrow) within the popliteal fossa and ruptured popliteal artery with pseudoaneurysm formation.
DISCUSSION
Non-typhoidal Salmonella are common food-borne infections that can result in bacteraemia and metastatic foci. Relapse has been described in 16.7% of patients with salmonellosis in one series[1], and factors associated with relapse include leucopenia, immunodeficiency, and with immunosuppressive therapy[1,2].
In a retrospective single-centre study of 129 patients, 39.5% had extraintestinal foci, the commonest of which is mycotic aneurysm, followed by pneumonia/empyema and spinal osteomyelitis. In this study, increasing age was the most significant risk factor for extraintestinal disease, which is in turn associated with higher mortality[3]. The commonest locations of non-typhoidal Salmonella mycotic aneurysms in the elderly include the abdominal aorta, followed by the thoracic aorta and then the iliofemoral artery[4]. Popliteal artery mycotic aneurysms secondary to non-typhoidal Salmonella (S. enteritidis being the most commonly implicated serovar) have been rarely reported in case reports, presenting predominantly with fever and leg swelling[5], as with our patient.
Important differentials in a patient presenting with fever and leg swelling include cellulitis, abscess, myositis, deep vein thrombosis, and haematoma. Owing to the potentially catastrophic risk of pulmonary embolism and due to its common occurrence, Duplex ultrasound is the commonest imaging modality of choice in the diagnostic evaluation of a patient with unilateral lower swelling. In our patient, we describe the clinical utility of MRI in the context of a patient presenting with bacteraemia with a microorganism with known propensity for causing endovascular infection.
Historically, open surgical repair and debridement is the treatment of choice in popliteal artery mycotic aneurysms. In recent years, endovascular methods are increasingly adopted. Riga et al. described five high-risk patients with peripheral infected aneurysms who were successfully treated by endovascular stenting[6]. Trellopoulos et al. reported the first case of a patient with S. enteritidis bacteraemia, who had spontaneous rupture of the popliteal artery and was successfully treated by endovascular repair with a covered stent[5]. To the best of our knowledge, our patient is the second reported case. Endovascular intervention is an attractive management option but the duration of antibiotics remains controversial in the setting of prosthetic endovascular grafts.