ABSTRACT
Introduction: Cerebral vasculitis is an uncommon life-threatening complication of community-acquired bacterial meningitis.
Patient and methods: We report the case of a 64-year-old woman with pneumococcal meningitis who developed parainfectious vasculitis causing ischaemic brain damage. Cerebral magnetic resonance imaging (MRI) confirmed the diagnosis. Clinical and radiological recovery after delayed addition of corticosteroid was achieved.
Discussion: This report shows that the onset of neurological deficits following pneumococcal meningitis can be caused by cerebral vasculitis. Underdosing with antibiotics and delayed adjunctive dexamethasone seem to favour this complication. There are no guidelines for treatment but high doses of steroids led to resolution in this case.
LEARNING POINTS
- Pneumococcal meningitis complicated by cerebral vasculitis can be treated with high-dose steroids.
- A repeat lumbar puncture is recommended to rule out relapsing or persistent infection in patients who deteriorate after 48 h of adequate antibiotic therapy.
- The cerebral vasculitis in our patient may have been caused by antibiotic underdosing and by delayed dexamethasone administration.
KEYWORDS
Cerebral vasculitis, pneumococcal meningitis, stroke, steroids
INTRODUCTION
Cerebral vasculitis is a rare life-threatening complication of community-acquired bacterial meningitis[1]. It is associated with a high mortality and a high incidence of neurological sequelae[2]. There is no standard treatment for this cerebrovascular complication but steroids are known to improve outcome[1].
CASE REPORT
A 64-year-old woman presented to a private hospital for headache and confusion after 1 week of neglected otalgia and fever. Physical examination showed neck stiffness, a Glasgow Coma Scale score of 14 and a temperature of 39°C. Lumbar puncture (LP) yielded cloudy cerebrospinal fluid (CSF): CSF white blood cells (WBC), 1,000/mm3; neutrophils, 76%; CSF protein, 1.95 g/l; CSF blood glucose ratio, 0.4. Gram staining revealed Gram-positive diplococci. The patient was diagnosed with pneumococcal meningitis. Treatment with cefotaxime 200 mg/kg/24 h was initiated within the first hour after initial medical contact with no associated dexamethasone. CSF culture isolated penicillin-resistant cefotaxime-susceptible Streptococcus pneumoniae. The minimal inhibitory concentrations were not available. Two hours later, the patient developed generalized seizures and acute respiratory failure managed with clonazepam and mechanical ventilation with sedation. A brain CT scan revealed no abnormalities.
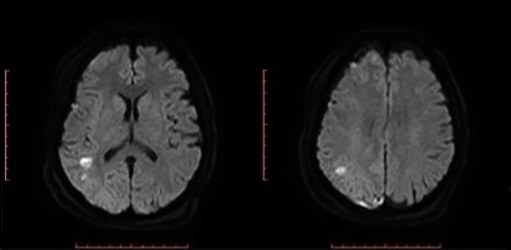
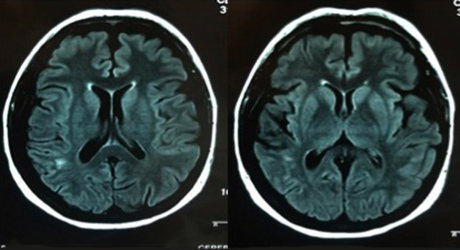
Three days later, the patient was referred to a tertiary intensive care unit (ICU) for persistent fever. On day 1 of ICU admission, she had recurrent generalized seizures. A second LP showed clear CSF: CSF WBC, <1/mm3; CSF protein, 0.5 g/l; CSF blood glucose ratio, 0.64. CSF culture was negative. Screening for other infections was negative. There were no signs of haemodynamic instability. The cefotaxime dose was increased to 300 mg/kg/24 h for a total of 14 days and adjunctive dexamethasone 10 mg four times daily for 4 days was initiated. By day 3 of this combination therapy, persistent apyrexia was obtained with no seizure recurrence. Consciousness was not affected after sedation was stopped, but neurological examination showed left proportional hemiplegia. Cerebral MRI showed multiple lesions with increased signal intensity in the right white matter of the parietal-insular and Rolandic areas (Fig. 1) and markedly restricted diffusion. These findings were consistent with infectious cerebral vasculitis. Methylprednisolone 1.5 mg/kg daily for 5 days was introduced and then replaced with oral prednisone 1 mg/kg daily for 2 months. The patient was discharged from the ICU on day 15. She remained in hospital and received physiotherapy until she recovered fully and left hospital on day 29. One month later, the patient had no complaints with complete regression of the neurological deficit. A follow-up cerebral MRI performed 2 months later showed subtotal regression of the subcortical parieto-insular right hypersignal (Fig. 2).
Figure 1. Diffusion-weighted sequence shows markedly restricted diffusion, as evidenced by the high signal intensity of the lesions.
Figure 2. Axial sequence T2 FLAIR shows regression of the abnormal subcortical parieto-insular right signal.
On each occasion, CT scan-guided chest drainage and intravenous antibiotics were required. Microbiological cultures were positive for endogenous anaerobic bacteria. The chest tube was finally withdrawn on day 62 leaving behind a localized persistent air-filled interstitial basal right-sided cyst (Fig. 1b). The patient was discharged from the ICU on day 72 under home ventilation.
Methods and Procedures
We searched PubMed using the keywords 'cerebral vasculitis', 'pneumococcal meningitis' and 'treatment'. Our search retrieved seven articles, five of which were case reports published between 2007 and 2017, that described four adult patients and three children. Empirical intravenous antibiotics with adjunctive dexamethasone were administered in all patients. Three patients completely recovered in 1–36 months, two had one or two long-term sequelae and two died after a few days[1–4].
DISCUSSION
We report one of the rare cases described in the literature of cerebral vasculitis following pneumococcal meningitis[1]. This cerebrovascular complication is not well understood and has a poor outcome with non-specific presentations; there are no guidelines for treatment.
Diagnosis of our case relied on the combination of persistent fever, recurrent generalized seizures, new onset of hemiplegia, normalized CSF parameters in the repeat LP and a normal CT cerebral scan. However, a repeat LP is now recommended to rule out relapsing or persistent infection in patients who deteriorate after 48 h of adequate antibiotic therapy[5]. A small number of patients with repeat LP have been diagnosed with delayed cerebral thrombosis after clinical deterioration. In these patients, CSF WBC remained elevated in contrast to our case. CSF bacterial cultures are commonly negative[4].
The discrepancy between clinical findings and a normalized repeat LP should prompt physicians to perform emergent brain MRI to rule out cerebrovascular complications including cerebral vasculitis. MRI has a sensitivity of over 90% for identifying cerebral vasculitis based on detection of white matter lesions, ischaemic necrosis and arterial changes, especially in the posterior area[1]. In the present case, the MRI findings were ischaemic lesions in the right white matter of the parietal-insular and Rolandic areas, explaining the left hemiplegia.
Two pathophysiological mechanisms for this complication are suggested. The first is an immune response affecting cerebral blood vessels resulting in delayed cerebral thrombosis. All patients in one study were treated initially with adjunctive dexamethasone, suggesting a dexamethasone-associated effect[4]. The main suggested mechanism is mediated by vascular inflammation due to proinflammatory cytokines and chemokines disrupting the blood–brain barrier following antibiotic-induced autolysis. Prompt use of intravenous antibiotics is key for the treatment of bacterial meningitis. A dosing regimen of 100 mg/kg/day of ceftriaxone, or 300 mg/kg/day of cefotaxime in case of penicillin-resistant Streptococcus pneumoniae, is recommended[5]. Adjunctive steroid treatment has shown its efficacy and is now indicated very early in the course of bacterial meningitis, before or at the time of the first dose of antibiotics[6]. In the present case, cefotaxime was initiated at a dosing regimen of 200 mg/kg/day for the 3 days after the first medical contact. The dose was then increased to the optimal dose. Adjunctive dexamethasone was introduced 3 days after the first antibiotic infusion. There were no reasons to suggest the vasculitis was due to cefotaxime underdosing and/or delayed adjunctive dexamethasone.
Several therapeutic schemes have been reported but data on the optimum duration of steroid administration are limited. In our patient, 2 mg/kg methylprednisolone for 5 days followed by tapering improved the deficit within 15 days[1]. High doses of steroids in other reports have been associated with immunosuppression. In the present case, 1.5 mg/kg methylprednisolone was initially used for 5 days, followed by 1 mg/kg prednisone for 2 months with progressive tapering leading to total resolution of the neurological deficit. The MRI findings had very nearly disappeared 2 months after the episode of meningitis.
In conclusion, this report shows that onset of neurological deficits following pneumococcal meningitis can be due to cerebral vasculitis, an uncommon but serious life-threatening complication. Inappropriate antibiotic dosing and delayed addition of dexamethasone seem to be risk factors for this complication. There are no guidelines for treatment, but high doses of steroids resulted in resolution of the neurological deficits in this case.