ABSTRACT
A 20-year-old asylum seeker presented with vomiting and left thigh pain, with a biological inflammatory syndrome. Pregnancy was diagnosed. Investigations revealed a pseudo-cystic, 20-cm-long retroperitoneal abscess, biopsy of which confirmed the diagnosis of tuberculosis. Evolution after cyst drainage and under conventional anti-tuberculosis treatment was favourable. An abdominal location of tuberculosis is rare and its diagnosis is difficult especially in countries with a low incidence of the disease. Unexplained abdominal manifestations and/or persistent biological inflammatory syndrome, especially in high-risk groups, should raise the suspicion of tuberculosis.
LEARNING POINTS
- Abdominal tuberculosis (TB) is a challenging diagnosis especially in low-incidence countries where the disease is rarely suspected.
- In low-incidence countries, abdominal TB should be suspected in cases of unexplained abdominal manifestations and/or persistent inflammatory syndrome, especially in high-risk groups.
- The diagnosis of abdominal TB is based on a range of anamnestic and clinical symptoms and signs, imaging, culture, and invasive procedures for histology.
KEYWORDS
Abdominal tuberculosis, inflammatory syndrome, pregnancy
CASE DESCRIPTION
A 20-year-old female Eritrean asylum seeker, who had arrived in Switzerland 6 months previously, presented to our primary care medicine department. She complained of nausea, vomiting and a pain in the left thigh of 15 days’ duration, without a history of trauma.
Physical examination was unremarkable except for tenderness on palpation of the left thigh. Biological tests revealed microcytic anaemia with a haemoglobin of 85 g/l (normal 120–160 g/l) and an MCV of 78 fl (normal 82–98 fl), an inflammatory syndrome with a CRP of 88 mg/l (normal 0–10 mg/l) and a sedimentation rate of 77 mm/h (normal 0–20 mm/h), and a slight disturbance of liver function with an ALP of 159 U/l (normal 25–102 U/l), GGT of 67 U/l (normal 9–35 U/l), and normal ASAT and ALAT. β-hCG was increased to 181,567 U/l.
Obstetrical ultrasound confirmed a 10-week pregnancy and the diagnosis of hyperemesis gravidarum was made. The woman was discharged.
To investigate the inflammatory syndrome, an extensive infection screen was performed including bacterial (blood, urine and stool cultures, brucellosis and syphilis serologies), viral (VZV, CMV, EBV, parvovirus B19, HTLV 1 and 2, measles, rubella, viral hepatitis and HIV) and parasitic (toxoplasmosis, leishmaniasis and malaria) screens. Tests confirmed past exposure to rubella, varicella and hepatitis A. The other tests were negative. The patient was also screened for TB: IGRA (QuantiFERON®-TB Gold) was positive, but chest X-ray was normal. Finally, the left thigh pain was investigated by an US scan of the soft parts of the thigh, which was normal.
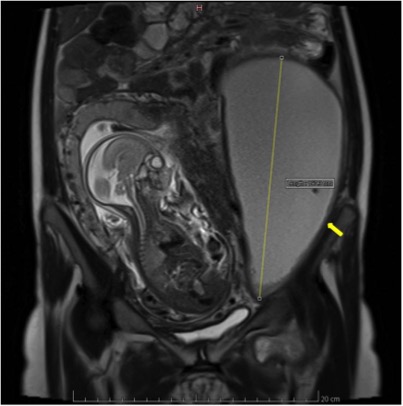
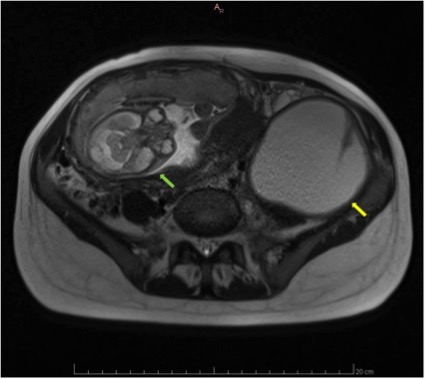
Abdominal and pelvic US performed at 20 weeks of amenorrhoea revealed a large left abdominal mass suggestive of an ovarian cyst, responsible for a left inguinal hernia. An MRI scan of the pelvis confirmed a left pseudo-cystic, 20-cm-long retroperitoneal abscess which extended along the left iliopsoas muscle and was associated with various tissue injuries along the left sympathetic chain (Figs. 1-3)
Figure 1 Sagittal section at 20 weeks of amenorrhoea showing the fetus facing the retroperitoneal mass (yellow arrow)
Figure 2. Cross-section at 20 weeks of amenorrhoea showing the fetus (green arrow) facing the retroperitoneal mass (yellow arrow)
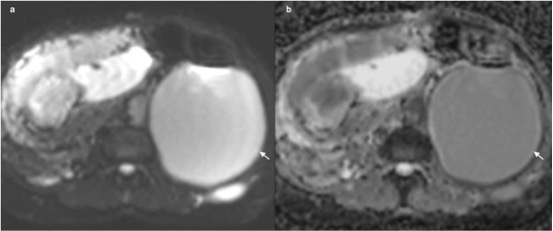
Figure 3. (a) Diffusion sequence b0 and (b) apparent diffusion coefficient (ADC) mapping. The axial plane in the upper abdomen shows ADC restriction (arrow on ‘a’), suggesting a tuberculosis collection. The denser or more cellular the biological tissue (e.g. pus), the less the diffusion of water and so the ADC. Low ADC appears in hypersignal on the diffusion sequence (a)
The radiological characteristics of the mass suggested a paraganglioma. However, a 24-hour urine and plasma fractionated metanephrines and catecholamines were normal, which excluded the diagnosis. Biopsy of the pseudo-cystic retroperitoneal abscess under US showed a granulomatous inflammation with giant cells, necrosis and acid-fast bacilli. PCR (GeneXpert) confirmed the diagnosis of TB.
A 14F catheter was inserted into the cyst and allowed drainage of about 3,000 ml of fluid over a few days. Conventional TB treatment (rifampicin, isoniazid, pyrazinamide and ethambutol) with fixed-dose combination tablets was started. No immunosuppressive factors or evidence of vertebral involvement were found. Evolution under treatment, and monthly monitoring by US, was favourable, with a transient and spontaneously reversible increase in liver tests.
Pregnancy was complicated by umbilical cord prolapse which required a caesarean section at 33 weeks of amenorrhoea. The patient gave birth to a healthy baby boy.
DISCUSSION
Abdominal TB represents about 6% of extra-pulmonary forms[1]. It can occur at any age with a peak frequency between 21 and 45 years of age[2]. The distribution by sex varies according to studies. A female predominance is observed in endemic countries, while a male predominance is reported in many European countries. This is explained by the larger percentage of males among immigrants, in whom abdominal TB is more frequent than among the local population[3]. The clinical manifestations of abdominal TB are extremely varied, which often results in a misleading picture and delayed diagnosis. Consequently, additional examinations are very important for correct diagnosis[2].
Peritoneal TB is the most frequent form of abdominal TB[1] which can also affect the gastro-intestinal tract, mesentery, abdominal lymph nodes, liver, spleen and pancreas[4]. However, there is no consensus definition of abdominal TB. TB of the genital and urinary systems, which is anatomically considered abdominal TB, is usually excluded from studies and guidelines for abdominal TB. This situation makes comparison between data from different studies difficult[5].
The treatment of abdominal TB is based on the same protocol as that for pulmonary TB with 2 months of quadritherapy, followed by 4 months of dual therapy[6]. Global mortality varies according to studies, ranging from 3% to 30% [2,7,8].
Pregnancy does not adversely impact the course of TB infection. However, it may mimic and mask the symptoms of early TB and thus delay its diagnosis[9]. Non-treated TB in the pregnant woman may lead to congenital TB in the infant. Comparative studies from India, Mexico and Taiwan found that infants born to mothers with TB have a two- to three-fold increased risk of neonatal complications such as prematurity and fetal growth retardation, as well as a six-fold increase in perinatal mortality[10–12]. The risk of transmission of TB to the infant is greater than the risks associated with TB treatment administered to the mother[9]. Therefore, treatment should be started whenever the probability of maternal disease is moderate to high. The treatment of a pregnant woman is the same as that of a non-pregnant woman[13]. Antituberculosis drugs do not have teratogenic effects in humans, even though they cross the placenta[13].
Many factors made the diagnosi s in this case challenging:
- Constitutional symptoms (fever, night sweats, fatigue and weight loss) were absent or hidden by the context of pregnancy (e.g. weight gain).
- There were no digestive symptoms, especially no abdominal pain, which is a usual symptom in 74–94% of patient [7,14] with abdominal TB.
- The main symptom on which we based our clinical reasoning was the inflammatory syndrome which is a frequent and non-specific sign.
- The patient had misleading symptoms such as the thigh pain due to the inguinal hernia or the hyperemesis gravidarum, which initially diverted the diagnosis.