ABSTRACT
Tuberculosis (TB) is an infectious disease caused by the Mycobacterium tuberculosis complex (MTBC). Pulmonary TB is the most common form of presentation, but extrapulmonary tuberculosis (EPTB) contributes significantly to morbidity and mortality. Rarely, patients with EPTB develop a form of ankle or foot arthritis. The diagnosis of TB arthritis is often overlooked because of the insidious onset and the non-specific clinical symptoms. Prognosis is generally poor; early diagnosis and delivery of the most appropriate treatment is critical to avoid functional disability.
LEARNING POINTS
- Tuberculous arthritis of the ankle has high morbidity but often goes undiagnosed.
- Tuberculous arthritis of the ankle can lead to degenerative changes in the bone and articular cartilage and even to joint collapse.
- Timely diagnosis and correct treatment are important to avoid functional disability.
KEYWORDS
Tuberculosis; extrapulmonary tuberculosis; osteoarticular tuberculosis; tuberculous arthritis; ankle arthritis
INTRODUCTION
Tuberculosis (TB) is an infectious disease caused by the Mycobacterium tuberculosis complex (MTBC) transmitted almost exclusively by cough aerosol. Although global TB incidence has slowly declined, it still remains a major health problem[1], accounting for 10.4 million new TB cases worldwide in 2015[2].
Pulmonary TB is the most common form of presentation, but extrapulmonary TB (EPTB) contributes significantly to morbidity and mortality, involving serous membranes, lymph nodes, the genitourinary tract, bowel, skeletal system and meninges. In particular, skeletal system involvement (osteoarticular TB) accounts for 2.2–4.7% of all TB cases and 10–15% of EPTB cases in Europe and the USA[3]. A very small number of people who have EPTB develop a form of ankle or foot arthritis which accounts for only 1–4% of all cases of osteoarticular TB[4]. We describe a case of ankle TB where timely diagnosis and appropriate treatment helped to avoid the worst outcome.
CASE REPORT
A 63-year-old woman was admitted to the Division of Internal Medicine at our institution complaining of a painful swelling of her left ankle. She reported that the swelling had gradually increased during the previous 7 months causing progressive limitation of movement with worsening in the preceding 4 weeks; no other symptoms were reported.
The patient had a medical history of arterial hypertension, chronic kidney disease stage 4 and chronic venous insufficiency.
Physical examination revealed a swollen and tender left ankle, without erythema or warmth. Foot and ankle movements and functions were difficult to evaluate because of the intense induced pain.
Laboratory findings on admission revealed an increased serum creatinine (2.72 mg/dl) and blood urea nitrogen (46 mg/dl), and a slight increase in erythrocyte sedimentation rate (39 mm/h) and C-reactive protein (7.4 mg/l). Other haematological parameters (serum electrolytes, liver enzymes, albumin, serum bilirubin), complete blood count and coagulation tests were normal. Rheumatoid factor level and autoantibodies tests were negative. A Quantiferon test was positive. Chest x-ray was negative for parenchymal alterations.
At foot x-ray (Fig. 1) it showed marked ankle osteoarthritis, with evidence of perimalleolar soft tissue swelling, periarticular calcifications and reduced bone mineral content. An ankle ultrasound showed soft tissue oedema and a fluid-encapsulated mass, with small solid inclusions, extending from the medial to the lateral malleolus.
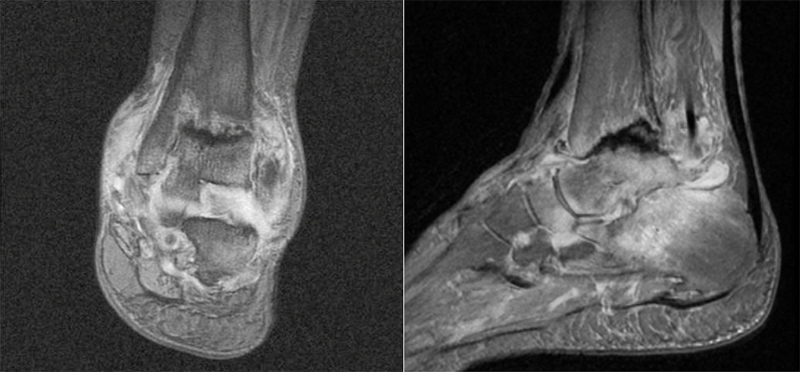
Because of the suspicion of infective arthritis, magnetic resonance imaging (MRI) of the foot and ankle was also performed (Fig. 2). The MRI documented hyper-intense thickening of the synovial membrane and structural alterations of the tibia, talus and calcaneus; several chondromatosis bodies in the anterior part of the tibiotalar joint were also detected.
Figure 1. An x-ray shows ankle osteoarthritis, with evidence of perimalleolar soft tissue swelling, periarticular calcifications and reduced bone mineral content
Figure 2.Magnetic resonance imaging shows hyper-intense thickening of the synovial membrane and structural alterations of the tibia, talus and calcaneus with several chondromatosis bodies in the anterior part of the tibiotalar joint
The patient underwent a longitudinal ankle joint incision (Fig. 3), medially to the anterior tibialis tendon, and the joint capsule was opened revealing an encapsulated mass. Once removed, it was sectioned on a Mayo table revealing a dense fluid content, similar to caseous necrosis.
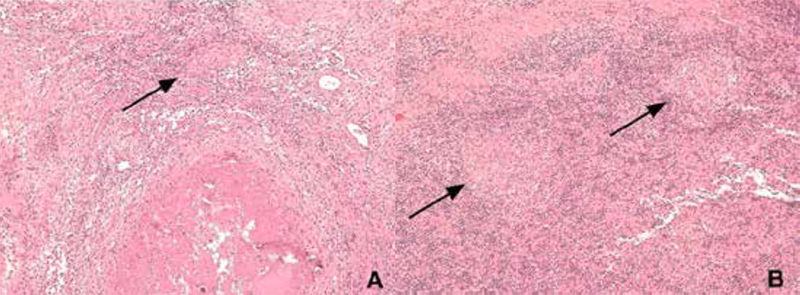
Culture tests and polymerase chain reaction (PCR) for MTBC were positive. The histopathological examination revealed a lesion mostly composed of large areas of necrosis surrounded by fibrous tissue where dense lymphocytic infiltrates were seen (Fig. 4A). Scattered granulomas were also present (Fig. 4B). Ziehl-Neelsen, Grocott and PAS staining did not reveal bacterial or fungal infection.
Figure 3. Longitudinal ankle joint incision
Figure 4. Histopathological features of the tibial lesion. The histopathological examination showed a lesion with large areas of necrosis (A) surrounded by fibrous tissue with dense lymphocytic (B) infiltrates and scattered granulomas (arrows)
Daily treatment with isoniazid 250 mg, rifampicin 600 mg, pyrazinamide 1500 mg and ethambutol 900 mg was started and continued for 2 months. Subsequently, treatment with isoniazid 250 mg and rifampicin 600 mg was continued for another 4 months. At follow-up, the patient showed improvement in pain and joint mobility.
DISCUSSION
Osteoarticular TB presents mainly as spondylodiscitis, arthritis and osteomyelitis. The spine is most commonly involved (50% of the cases), but the hips and knees can also be affected. A very small number of patients with osteoarticular TB develop a form of ankle or foot arthritis[4]. TB joint involvement can mimic a wide range of acute and chronic conditions like infectious or septic osteomyelitis, inflammatory arthritis, osteochondrosis, Charcot arthropathy, or bone or soft tissue tumours.
Tuberculous arthritis is usually 'cold’, which means that there is no erythema and the skin over the infected joint is the same temperature as normal skin. The most common symptoms of TB of ankle joint involvement are pain, swelling, limited range of motion, bone tenderness, limping and muscle spasms. Inguinal lymphadenopathy or systemic manifestations such as fever, night sweats, malaise, anorexia and weight loss may also be present. At a more advanced stage, there might be complete joint degeneration and ankylosis. From a clinical point of view, it is therefore essential to highlight that tuberculous arthritis should be considered in the differential diagnosis of arthritis in a ‘cold’ joint.
Ankle x-ray imaging is an important first step in the diagnostic work-up as it usually documents juxta-articular bone loss, peripheral osseous erosions and gradual reduction of joint space. Typically, the lytic areas of destruction and erosions are seen along the articular margins. In the initial stages of the disease, there is relative preservation of the joint space, differently from septic arthritis, while at more advanced stages joint destruction, sclerosis and fibrous ankylosis are present[5]. An MRI examination can be useful especially to more precisely define bone and soft tissue involvement. As a general rule, a definitive diagnosis of bone involvement is achieved from open biopsy, with subsequent isolation of MTBC in standard culture or by DNA amplification with PCR. It is important to note that osteoarticular TB is a paucibacillary lesion and as such, acid-fast bacilli in cultures from the lesions are seldom found. Thus, molecular diagnostics are a reliable alternative diagnostic tool[5].
Pharmacological therapy is the mainstay of treatment. The approach is the same as that for active pulmonary TB: 6 months of isoniazid and rifampicin including supplementation with pyrazinamide and ethambutol for the first 2 months. Surgery should be reserved for those patients without clinical response to medical therapy. Procedures like sequestrectomy and debridement are the most commonly performed and may decrease infectious load and encourage early recovery[6].
In the described case, we confirm – as already highlighted in a case series[5] – that the diagnosis of tuberculous arthritis of the ankle is first based on clinical suspicion, which is key for quickly initiating appropriate diagnostic investigations.
In conclusion, tuberculous arthritis of the ankle is a rare entity with high morbidity. The diagnosis is often overlooked because of insidious onset and aspecific clinical symptoms. Since bone lesions increase in size and provoke degenerative changes of the articular cartilage, until joint collapse, early identification is critical for successful treatment and to avoid permanent functional disability.