ABSTRACT
Primary hepatic lymphoma (PHL) is a rare variant of non-Hodgkin's lymphoma. Diffuse hepatic involvement is uncommon and therefore presentation as progressive hepatitis or acute fulminant hepatic failure is rare. Acute onset of signs and symptoms can mimic a variety of infectious and inflammatory disorders, thus delaying the diagnosis. A high index of suspicion and liver biopsy early in the course of liver dysfunction may establish the diagnosis and allow rapid initiation of chemotherapy to prevent a fatal outcome. In this report, we describe a rare case of fulminant primary hepatic diffuse large B-cell lymphoma in a 55-year-old woman who died 2 weeks after admission, before the initiation of chemotherapy.
LEARNING POINTS
- Primary hepatic lymphoma (PHL) is a rare yet serious disease which should be suspected in every case presenting as hepatitis with unclear aetiology.
- A liver biopsy should be performed as early as possible when PHL is suspected.
- Failure to detect PHL early can result in rapid deterioration and death within 2 weeks of presentation.
KEYWORDS
Primary hepatic lymphoma, non-Hodgkin’s lymphoma, diffuse large B-cell lymphoma, acute fulminant hepatitis
CASE REPORT
A 55-year-old Lebanese woman was admitted to our hospital after 3 weeks of intermittent fever, chills, diffuse myalgia and arthralgia, mild epigastric discomfort, nausea and vomiting, but no weight loss or night sweats. Her past medical history was only remarkable for cholecystectomy at the age of 40. On examination, her temperature was 38.0°C and she was slightly icteric. Her liver was enlarged, firm and tender; no splenomegaly or enlarged lymph nodes were noted.
Laboratory results were within the normal range apart from an ESR of 89/h, CRP of 150 mg/l, Hb of 11.6 g/dl, WBC of 23,000/μl and elevated liver function tests: total bilirubin 2.3 mg/dl, direct bilirubin 1.5 mg/dl, AST 289 U/l, ALT 380 U/l, INR 1.2, lactate dehydrogenase (LDH) 923 U/l, alkaline phosphatase 464 U/l and gamma glutamyl transferase 1089 U/l. Serology tests for hepatitis A, B and C, CMV, EBV, HIV, brucellosis and typhoid fever were normal. Six blood cultures and a urine culture were negative. The PPD skin test was negative. Beta-2 microglobulin levels were normal. ANA and RF were negative, and anti-smooth muscle and anti-mitochondrial antibodies were negative; CEA, CA 19-9 and AFP levels were normal. Blood and urine immunoglobulin levels were also normal.
Abdominal ultrasound, a computed tomography (CT) scan of the abdomen and MRCP revealed only diffuse hepatomegaly without portal or hepatic vein thrombosis. A chest CT scan and gastroscopy were normal.
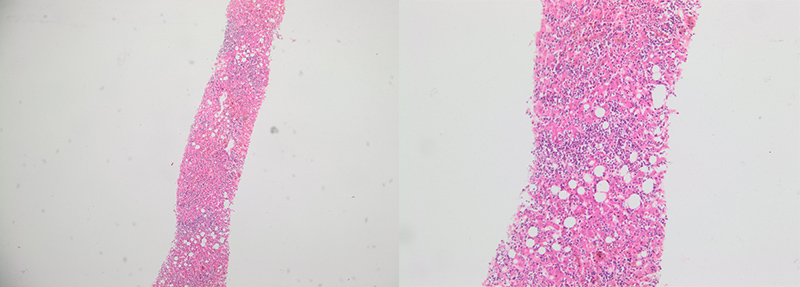
Bone marrow biopsy demonstrated only mild hypercellularity. A core liver biopsy showed heavy infiltration mainly of large lymphoid cells (Fig. 1). The cells were positive for CD20 and LCA, indicating a diagnosis of diffuse large B-cell lymphoma according to the WHO classification. The proliferation index was very high with 80% of the cells Ki-67 positive. Since there were no other foci of lymphoma, the patient was diagnosed with extra-nodal lymphoma that originated in the liver.
As the patient developed worsening haemolytic anaemia and thrombocytopenia (Hb 8.8 g/dl, platelets 44,000/μl, LDH 2,500 U/l), steroids (2 mg/kg/day) and broad-spectrum antibiotics were started.
After an initial improvement, liver function worsened (bilirubin 70 mg/dl) and haemoglobin dropped to 6.8 g/dl. The patient developed acute respiratory distress syndrome with severe lactic acidosis and died 2 days after diagnosis, 2 weeks following admission, before any chemotherapy.
Figure 1. Core liver biopsy showing heavy infiltration mainly of large lymphoid cells
DISCUSSION
Non-Hodgkin’s lymphoma is a common lympho-proliferative disease; liver involvement occurs in 10% of patients. Primary hepatic lymphoma (PHL) is an extra-nodal lymphoma of the liver without involvement of any other organ (lymph nodes, spleen, etc.). PHL is notably rare, representing <1% of all extra nodal lymphomas[1,2]. The vast majority of PHL patients present with signs and symptoms mimicking acute hepatitis and constitutional symptoms[2] which may delay the diagnosis. Hepatomegaly is found in most patients (75–100%), B symptoms (fever, drenching sweats and weight loss) in 37–86%, weight loss in 57% and jaundice in 4 [1,3]. PHL may present as a solitary liver mass (42%) or as multiple lesions (50%); diffuse infiltration of the liver is rare in Caucasians (8%)[1].
Patients with PHL have elevated LDH and liver function tests, mostly alkaline phosphatase
The predominant histology of PHL is diffuse large B-cell lymphoma (DLCL)[2,3], as was the case for our patient; a few cases of small lymphocytic[3], histiocytic, follicular[1,6] T-cell[3,7] and other types have also been described.
Our patient presented with clinical and laboratory features which were not highly suggestive of PHL. Liver biopsy with specific immuno-histochemistry was the only test to confirm the diagnosis.
The prognosis of PHL is poor (median survival of 6 months) for patients treated with chemotherapy alone, but better for patients treated with a combination of modalities (8–16 months)[8,9]. Massive liver infiltration, a high index of proliferation, and elevated LDH levels (all present in our patient), as well as advanced age, cirrhosis and elevated levels of beta-2 microglobulin, are worse prognostic factors[3,4].
It is important to recognize that in rare circumstances, PHL can present with fulminant hepatic failure, and because of the ambiguous features and rapid progression, most cases are diagnosed on autopsy with an average survival of 10.7 days from diagnosis[10]. In our case, the patient died 2 weeks after hospital admission.
In conclusion, PHL, although a rare disease, should be considered in any patient of any age who presents with unexplained progressive hepatitis, acute hepatic failure, liver mass or diffuse infiltration.
If the clinical picture is suspicious for PHL, a liver biopsy should be obtained early because rapid progression can cause fulminant hepatic failure and refractory coagulopathy. Furthermore, early detection of PHL and timely initiation of the new multi-agent chemotherapy and the addition of rituximab may offer an appropriate treatment with a very good response[3].