ABSTRACT
Takotsubo cardiomyopathy is a condition characterized by transient left ventricular systolic and diastolic dysfunction, with a possible direct causal role of catecholamine in its pathophysiology. We present a case of a woman with shock and adrenal insufficiency in whom Takotsubo cardiomyopathy developed after treatment with norepinephrine. This case confirms the direct causal role of catecholamine in the pathophysiology of Takotsubo cardiomyopathy. An 82-year-old woman presented with asthenia, anorexia, nausea and abdominal pain. The patient had been on chronic corticosteroid therapy until 3 months before, when she underwent abdominal surgery and corticosteroids were stopped. She now presented with acute kidney injury, hyponatremia and hyperkalemia and shock. A norepinephrine continuous infusion was administered to maintain a mean arterial pressure over 65 mmHg. An echocardiogram showed severe hypokinesis in the apical segments and hyperdynamic basal segments, with an ejection fraction of 25%. Plasma cortisol level was 4.5 µg/dL (reference range 5-25). Corticosteroid therapy was begun and norepinephrine was tapered and stopped. A new echocardiogram showed normalization of cardiac wall motion and an ejection fraction of 70%. This case highlights the importance of the correction of the cause of shock, as well as the risks associated with the use of norepinephrine if hypotension is severe or if it persists despite fluid administration, as usually recommended. It also confirms the direct causal role of catecholamine in the pathophysiology of Takotsubo cardiomyopathy. To the best of our knowledge, this is the first report of stress-induced cardiomyopathy secondary to norepinephrine by continuous infusion for shock.
LEARNING POINTS
- Takotsubo cardiomyopathy is a condition characterized by transient left ventricular dysfunction of the apex and midventricle in the absence of attributable coronary artery disease.
- In patients with shock and adrenal insufficiency, who can be erroneously interpreted as septic shock, Takotsubo cardiomyopathy can develop after treatment with norepinephrine.
- In the management of shock, there are risks associated with recommending the use of norepinephrine if hypotension is severe or if it persists despite fluid administration, when the cause of shock is other than septic shock and is not corrected.
- There is a direct causal role of catecholamine in the pathophysiology of Takotsubo cardiomyopathy.
KEYWORDS
Shock, Takotsubo cardiomyopathy, adrenal insufficiency, norepinephrine, vasoconstrictor agents, vasoactive agents
INTRODUCTION
akotsubo cardiomyopathy, also called apical ballooning syndrome or stress cardiomyopathy, is a condition characterized by transient left ventricular systolic and diastolic dysfunction of the apex and midventricle in the absence of attributable coronary artery disease. It typically occurs in postmenopausal women and may be preceded by a stressful or emotional event[1]. We report a case of Takotsubo cardiomyopathy induced by norepinephrine continuous infusion in a patient with shock caused by adrenal crisis, erroneously interpreted as septic shock.
CASE REPORT
An 82-year-old woman presented with asthenia, anorexia, nausea and abdominal pain. Five years earlier, a diagnosis of systemic lupus erythematosus had been made[2] and therapy with daily prednisolone 17.5 mg and azathioprine 50 mg started.
Three months before the present episode, the patient underwent emergency surgery for a small bowel obstruction, caused by a transmural necrosis of the colon adjacent to an ileocolic anastomosis (performed 20 years earlier for adenocarcinoma of the cecum). An ileocolic resection and an ileostomy were performed. The patient had an uneventful recovery and was discharged after 9 days. Two days after discharge, the patient was readmitted due to dehydration and acute kidney injury, as a result of an overactive ileostomy. No corticosteroids or other immunosuppressants were administered during both episodes.
During the next month, there were no new medical events, until 24 hours before this admission, when asthenia, anorexia, nausea and abdominal pain occurred and the patient presented to the emergency department the next day. The patient had a history of hypertension, aortic stenosis, hypothyroidism, depression and osteoarthrosis of the hip and knee. Medications were enalapril, amiloride/hydrochlorothiazide, levothyroxine, sertraline, clopidogrel, and chondroitin.
On examination, her temperature was 35.6 °C; pulse 89 beats per minute; and blood pressure 90/59 mmHg. Oxygen saturation was 99% at room air and she had diffuse abdominal tenderness. The remainder of the examination was normal.
Laboratory work was remarkable for thrombocytopenia (52,000/uL), leukocytosis and neutrophilia (13,100/uL and 11,300/uL, respectively) with an undetectable C-reactive protein (<0.5 mg/dL). There was acute kidney injury (creatinine 2.53 mg/dL) with hyponatremia (sodium 124 mmol/L) and hyperkalemia (potassium 5.9 mmol/L) and a serum lipase of 1185 U/L (normal range <300 U/L).
Arterial blood gas analysis, at room air, included a pH of 7.27 (reference range 7.35-7.45); a partial pressure of carbon dioxide of 20 mmHg (reference range 32-45); a partial pressure of oxygen of 108 mmHg (reference range 83-108); a bicarbonate level of 9 mmol/L (reference range 21-28); and a lactate of 2.2 mmol/L (reference range 0.5-1.6). An abdominal ultrasound showed multiple gallstones, without other sonographic criteria for acute cholecystitis, with no evidence of dilated intrahepatic ducts or the common hepatic duct; the pancreas was normal in appearance (partially visualized due to overlying bowel gas) with no ascites.
Fluid loading began with a balanced salt solution. The patient became prostrate, with a blood pressure of 87/52 mmHg and was admitted to the intensive care unit (ICU). In the ICU, the patient maintained a mean arterial pressure under 50 mmHg and a continuous infusion of norepinephrine was administered, with a rate of 0.8 µg/kg/min to obtain a mean arterial pressure over 65 mmHg. Plasma adrenocorticotropic hormone (ACTH) levels were 8 ng/L (reference range 6-76) and plasma cortisol levels were 4.5 µg/dL (reference range 5-25). Methylprednisolone was started 40 mg twice daily, and norepinephrine dose tapering was possible.
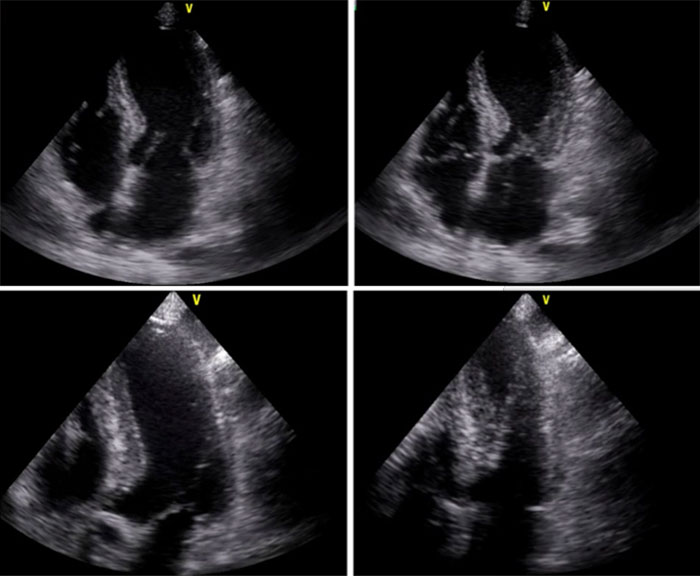
A transthoracic echocardiogram (while on 0.5 µg/kg/min norepinephrine) showed severe hypokinesis in the apical segments and hyperdynamic basal segments, with an ejection fraction of 25% (Video 1, Fig. 1). There was a troponin-I peak of 1.72 ng/mL on day 3 of admission to ICU. Methylprednisolone was substituted for prednisolone 20 mg and norepinephrine tapering was continued, until it was stopped 48 hours after the echocardiogram was performed. Piperacillin/tazobactam was administered for 4 days, with a peak procalcitonin of 0.55 ng/mL. Blood and urine cultures were negative, and lipase levels became normal within 48 hours, with no abdominal pain. The patient was transferred to the general internal medicine ward on day 5 of admission to ICU, where a new echocardiogram showed normalization of cardiac wall motion and an ejection fraction of 70% (Video 2, Fig. 1). The patient was discharged on day 11 of admission.
Figure 1. (a) First echocardiogram: diastole with norepinephrine. (b) First echocardiogram: systole with norepinephrine (ejection fraction 25%, velocity time integral (VTI) 13 cm). (c) Second echocardiogram: diastole without norepinephrine. (d) Second echocardiogram: systole without norepinephrine (ejection fraction 70%, VTI 20 cm).
Video 1 (click to enlarge)
Video 2 (click to enlarge)
Video 1. First echocardiogram: severe hypokinesis in the apical segments and hyperdynamic basal segments, with an ejection fraction of 25%.
Video 2. Second echocardiogram: normalization of cardiac wall motion and an ejection fraction of 70%.
DISCUSSION
We present a case of a patient with shock and adrenal insufficiency, in whom Takotsubo cardiomyopathy developed after treatment with norepinephrine. Although some animal studies show Takotsubo cardiomyopathy induced by norepinephrine infusion[3,4], we found only a single case report in human patients with a Takotsubo cardiomyopathy secondary to iatrogenic norepinephrine injection[5]. In that article, Takotsubo cardiomyopathy was induced by a single 4 mg norepinephrine injection. Our case is more complex, not only because Takotsubo cardiomyopathy was induced by continuous infusion of norepinephrine, but also because adrenal insufficiency had to be corrected.
Alternatively, this case might be interpreted as an acute pancreatitis with septic shock and multiple organ failure, including adrenal insufficiency. Nevertheless, this scenario would not explain the severe apical hypokinesis with hyperdynamic basal segments, as well as its normalization within a few days. The rapid recovery of the multiple organ failure, normalization of the elevated lipase (in 48 hours) and tapering off of the norepinephrine infusion (immediately after corticosteroid administration) also do not favor the diagnosis of acute pancreatitis with septic shock and multiple organ failure.
Best practice in the management of shock recommends using norepinephrine if hypotension is severe or if it persists despite fluid administration[6]. It is also recommended that treatment should include correction of the cause of shock and hemodynamic stabilization, primarily through fluid infusion and administration of vasoactive agents. This case report highlights the importance of the former and the risks of the latter, and confirms the direct causal role of catecholamine in the pathophysiology of Takotsubo cardiomyopathy. To the best of our knowledge, it is the first report of stress-induced cardiomyopathy secondary to norepinephrine by continuous infusion for shock.
CONCLUSION
When managing patients in shock and before starting vasoactive agents, one should always think of possible causes of shock, including adrenal insufficiency, as inappropriate norepinephrine infusion might have a causal role in the development of a Takotsubo cardiomyopathy.