ABSTRACT
Pulmonary embolism (PE) is the most serious and life-threatening clinical presentation of venous thromboembolism, and difficult to diagnose. Triple point-of-care-ultrasonography (POCUS) of the lung, heart and leg veins is a multiorgan approach that may help to evaluate patients suspected of having PE, in combination with existing protocols and computed tomographic pulmonary angiography (CTPA). We present the case of a 26-year-old man with sudden onset of dyspnoea and swelling of the leg with a Well’s score of 9. With CTPA unavailable at the time of presentation, triple POCUS showed subpleural consolidations and a venous thrombus in a popliteal vein. A diagnosis of deep vein thrombosis with PE was made and the appropriate treatment was started immediately. Although triple POCUS has less sensitivity and specificity than CTPA, it could be very useful in some clinical settings.
LEARNING POINTS
- In a patient with suspected pulmonary embolism, the best diagnostic strategy is to combine clinical assessment, plasma D-dimer measurement and computed tomographic pulmonary angiography (CTPA).
- Triple point-of-care ultrasonography of the lung, heart and leg veins may improve clinical assessment of pulmonary embolism if CTPA is unavailable or contraindicated.
- Point-of-care ultrasonography should be incorporated as the fifth pillar of the physical examination.
KEYWORDS
Point-of-care ultrasonography, pulmonary embolism, deep vein thrombosis, triple POCUS
INTRODUCTION
Venous thromboembolism (VTE) is a major health problem, with an overall annual incidence of between 100 and 200 per 100,000 inhabitants[1]. Pulmonary embolism (PE) is the most serious and life-threatening clinical presentation of VTE, and difficult to diagnose[2]. The European Society of Cardiology suggests that the best diagnostic strategy to confirm or exclude PE is to combine clinical assessment, plasma D-dimer measurement and computed tomographic pulmonary angiography (CTPA)[3]. Nowadays, the gold standard for making a diagnosis is CTPA, but this technique has some limitations such as high cost, unsuitability for unstable patients, and lack of 24-hour availability in some institutions, and is contraindicated in patients with renal failure or contrast allergy and in pregnant women[4,5].
Triple point-of-care-ultrasonography (POCUS) of the lung, heart and leg veins is a multiorgan protocol proposed as a new tool to evaluate patients suspected of having PE. The idea of single organ evaluation for the diagnosis of PE was studied previously[6,7], but low sensitivity and specificity have limited its clinical application. Nazerian et al. were the first to test the multiorgan approach, and the results were very encouraging with a high sensitivity (82.8–94.9%) and negative predictive value (91.4–97.5%)[4]. That led to some algorithms integrating triple POCUS with Well’s score and the D-dimer test to increase the pre-test probability of PE, and better select patients for CTPA[5]. In this case report, we discuss the triple POCUS approach for the diagnosis of PE, balancing its sensitivity and specificity with its potential to enhance the traditional physical examination.
CASE DESCRIPTION
We present the case of a 26-year-old man with no previous medical history or and not on chronic medication. He was being treated for an upper airway infection with levofloxacin 500 mg once a day and ibuprofen 600 mg three times a day and had been on bedrest for the previous 3 days. He presented to the emergency department with a sudden onset of dyspnoea associated with a stabbing pain in the left hemithorax that aggravated with deep inspiration. The pain woke him in the middle of the night, and he felt tired and fatigued when he tried to walk. He denied fever, cough or purulent sputum. He had a respiratory rate of 24 breaths per minute with peripheral oxygen saturation of 92%, blood pressure of 138/79 mmHg and heart rate of 115 bpm. Chest auscultation revealed crepitations at the lower left lung base and rhythmic cardiac sounds without murmurs. There was noticeable swelling of the right leg that had been getting worse since the patient woke up, and the foot was warm and had normal colouration with the dorsalis pedis arterial pulse present. At this time, PE was the most probable diagnosis, with a calculated Well’s score of 9 points (clinical signs and symptoms of deep vein thrombosis (DVT), 3 points; PE the most probable diagnosis, 3 points; heart rate >100, 1.5 points; immobilization for the last 3 days, 1.5 points; high-risk group for PE, pre-test probability of 40.6%). Laboratory analysis of blood showed pH 7.42, PaO2 62 mmHg, PaCO2 32 mmHg, HCO3– 24.4 mmol/l, SatO2 92.4%, and lactates 0.8 mg/dl. A chest x-ray did not show any significant abnormality and ECG demonstrated a sinus rhythm with a heart rate of 118 bpm. Laboratory evaluation showed leukocytes in the normal range (6.3×109/l) and a slightly elevated C-reactive protein (1.44 mg/dl). CPTA was not available at the time of presentation, so the triple POCUS protocol was applied as follows:
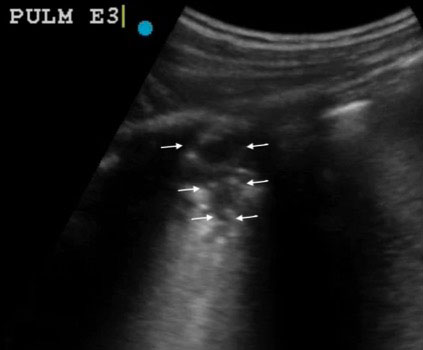
- i) For pulmonary ultrasonography we followed the SLESS protocol (six-field evaluation)[8]. An ‘A’ pattern was observed on all right lung fields, while on the left lung an ‘A’ pattern was observed on the apex, but some ‘B’ lines were seen in the anterior part of the lung base and a small sub-pleural consolidation was seen in a more posterior position (Fig. 1).
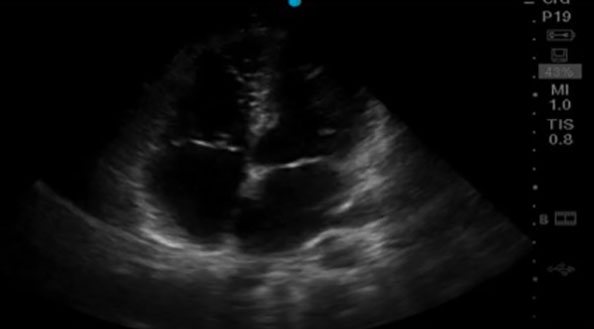
- ii) Cardiac evaluation did not show dilation of the right chambers or any thrombi (Fig. 2).
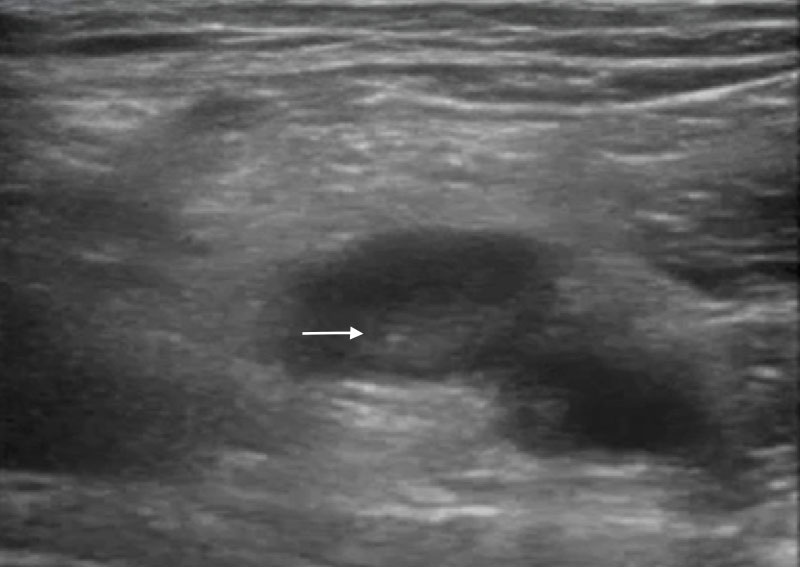
- iii) Evaluation of the leg veins showed a right popliteal thrombus; all other evaluated zones had a normal compression test (Fig. 3).
The finding of a lower leg DVT associated with a probable lung infarction confirmed our strong suspicion of PE. Treatment was immediately started with enoxaparin 1 mg/kg twice a day. The next day the patient underwent a CTPA which showed pulmonary artery filling faults and a small triangular-shaped consolidation in the left base compatible with pulmonary infarction. An echo-Doppler of the lower limbs confirmed the presence of a thrombus in the right popliteal vein. The patient recovered quickly and was discharged 3 days after admission.
Figure 1. Sub-pleural triangular consolidation (arrows) on the left lung, corresponding to pulmonary infarction
Figure 2. Apical four-chamber view without right heart enlargement
Figure 3. Thrombus in the right popliteal vein (arrow), resulting in a non-compressible vein
DISCUSSION
This case highlights the importance of POCUS for physical examination and the promise of triple POCUS for evaluating patients suspected of having PE. When CTPA was not available, POCUS evaluation allowed us to make a diagnosis of PE and start treatment immediately. However, triple POCUS is less sensitive and less specific than CTPA which is usually readily available and is to be preferred for diagnosing PE. Nevertheless, POCUS can be used to enhance the physical examination and confirm the suspected diagnosis. We suggest that POCUS should be the fifth pillar of the physical examination[9].