ABSTRACT
A 57-year-old woman, with a history of deep venous thrombosis and medicated with warfarin, presented at the hospital with acute back pain with paraplegia, headache, high blood pressure and vomiting. Imaging of the spine showed an acute intradural extramedullary haemorrhage with blood clot formation. The patient underwent surgery and received intensive post-surgical physiotherapy but remains paraplegic. Non-traumatic spinal intradural extramedullary haematoma (SIEH) is a rare neurological emergency that can result in spinal cord compression. Physicians should always consider this clinical entity as a differential diagnosis, especially in a patient presenting with acute back pain on anticoagulant therapy.
LEARNING POINTS
- Non-traumatic spinal intradural extramedullary haematoma is extremely rare.
- Acute cases can lead to spinal cord compression.
- Physicians should consider this clinical entity in anticoagulated patients presenting with acute onset of back or radicular pain followed by paraplegia, intestinal and bladder dysfunction.
KEYWORDS
Spinal intradural extramedullary haematoma, spinal subdural haematoma, anticoagulation
INTRODUCTION
Non-traumatic spinal intradural extramedullary haematoma (SIEH), without underlying pathological changes, is an extremely rare emergency which can result in spinal cord compression. SIEH should be suspected in patients presenting with a history of back or radicular pain followed by paraplegia, intestinal and bladder dysfunction[1]. Causes include iatrogenic medical procedures (spinal anaesthesia or punctures), use of anticoagulants, bleeding disorders (haemophilia, leukaemia and thrombocytopenia), vascular lesions and neoplasms[1,2].
CASE REPORT
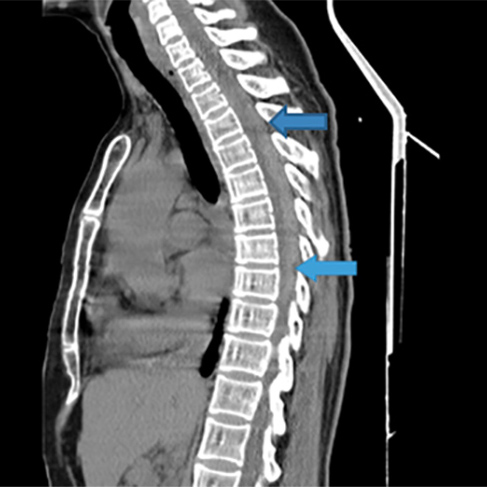
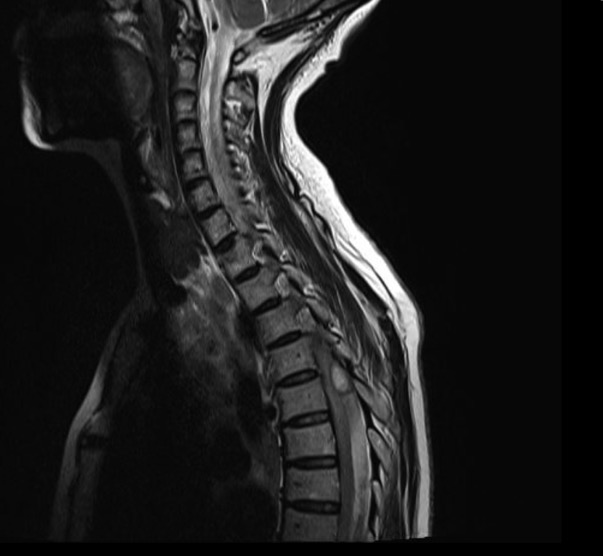
A previously healthy 57-year-old woman, with a known history of deep venous thrombosis and on medication with warfarin for the previous 2 years, arrived at the emergency department of our district hospital with a 1-day history of acute back pain of the cervical, thoracic and lumbar segments, headache, self-measured high blood pressure and vomiting. Measurement of vital signs revealed high blood pressure of 141/92 mmHg, tachycardia of 110 bpm and no fever. Clinical examination revealed normal muscle strength (5/5) in the upper extremities and grade 0/5 in the lower extremities with urinary retention which required bladder catheterization. There were no meningeal signs. Blood analysis revealed elevated values of creatinine (2.2 mg/dl), C-reactive protein (1.20 mg/dl), prothrombin time (PT 94.80 seconds) and International Normalized Ratio (INR 6.67) for which vitamin K was administered. Computed tomography (CT) of the head was normal. CT of the spine revealed a slightly hyperintense intradural lesion at the T4–T8 level with spinal cord compression (Fig. 1). Magnetic resonance imaging (MRI) of the spine showed an acute intradural extramedullary haemorrhage with blood clot formation. (Fig. 2).
Figure 1. Initial CT scan with a suggestion of intradural hyperintensity between T4 and T8 (between arrows) with probable compression and deviation of the spinal cord
Figure 2. Spinal MRI showing intradural extramedullary haemorrhage at T4–T8
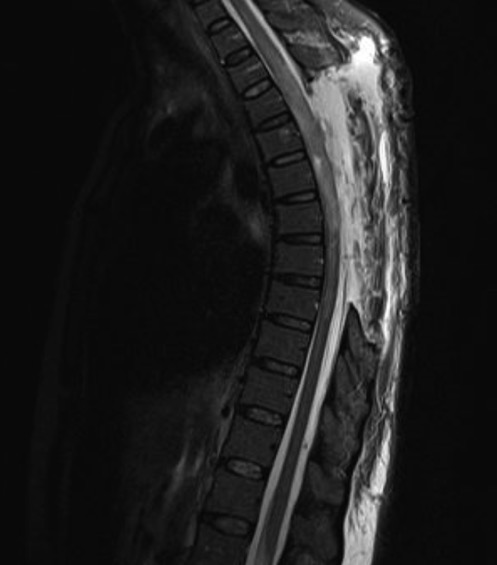
The patient was transferred to a central hospital and underwent bilateral laminectomy with median durotomy and removal of a compressive and voluminous acute subdural haematoma. MRI was repeated 1 week after surgery because of dorsal back pain, and demonstrated a retro-thecal pseudo meningocele extending to the retro-vertebral muscular layers, subcutaneous tissue with a fistula extending to the skin on the right side at the T1–T2 level, and medullary oedema from T3 to T9 (Fig. 3). The patient was transferred back to the Internal Medicine ward for further care where she received intensive physiotherapy for 3 months before finally securing a place at a specialized rehabilitation centre. At 6 months after hospital discharge, she remains paraplegic with bowel and urinary dysfunction.
Figure 3. MRI image 1 week after surgery showing a retro-thecal pseudo meningocele extending to the retro-vertebral muscular layers, subcutaneous tissue with a fistula extending to the skin on the right side at the T1–T2 level, and medullary oedema from T3 to T9
DISCUSSION
IEHs normally present with a mixed subdural and subarachnoid location[2]. The less defined anatomical areas of the spine make it difficult to distinguish among a subdural, a subarachnoid and a mixed bleeding pattern, and thus the scientific term "intradural extramedullary haematoma" was devised[1].
SIEHs are often located in the thoracic and thoracolumbar region[2]. In terms of gender predominance, females show a major peak of incidence of non-traumatic spontaneous acute spinal subdural haematomas over the age of 60 years, when vascular pathologies are frequent and anticoagulation therapy is used widely for treatment[3].
In patients presenting with abrupt back pain with or without radicular pain with accompanying neurological symptoms, a careful clinical history covering the above causes of SIEH is important in preventing irreversible paralysis[4]. MRI is the gold standard of imaging diagnosis[4]. Treatment consists of haematoma evacuation by surgery, although there is some preference for conservative treatment in patients with mild neurological symptoms[1]. Physicians, especially internists, should be able to quickly recognize this neurological emergency, especially in a patient on anticoagulant therapy, as we deal with so many differential diagnoses of back pain in the Emergency Room[5].