ABSTRACT
We describe a case of emphysematous pancreatitis, a rare and serious complication of acute pancreatitis, which has a high mortality rate.
LEARNING POINTS
- The development of emphysematous pancreatitis implies the existence of infected necrosis.
- It is characterized by the replacement of the pancreatic bed by gas presence.
- The development of endoscopic techniques represents a promising advance in the treatment of this condition.
KEYWORDS
Emphysematous pancreatitis, pancreatic necrosectomy, necrotizing pancreatitis
CASE DESCRIPTION
A 63-year-old hypertensive, male ex-smoker with chronic gastritis and a history of duodenal ulcers, presented to our centre with abdominal pain and malaise. The physical examination revealed pain in the mesogastrium without peritonism. Blood analysis showed amylase of 1,640 U/l, lipase 47,480 and leucocytosis 17,020. Coagulation was normal. An abdominal x-ray showed a distended intestinal loop in the right/central part of the abdomen (sentinel loop sign), abundant fecaloid remains in the colon, and the upper end of the left psoas muscle that appeared erased, the right renal silhouette was not visible (Fig. 1).
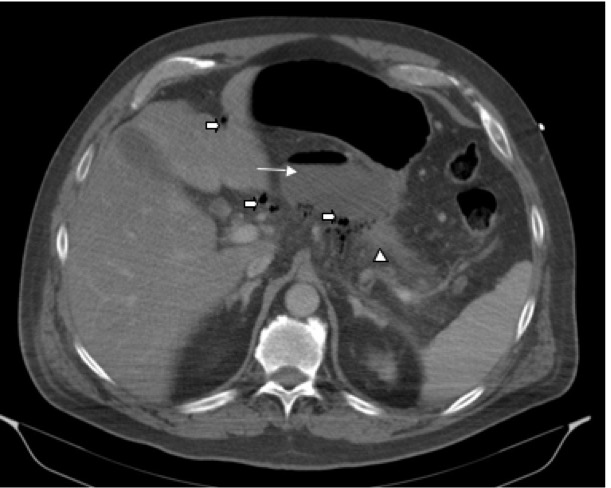
The patient was admitted with a diagnosis of acute pancreatitis. The evolution was initially favourable, but there was sudden clinical worsening 48 hours after admission with intense pain, fever and hypotension. A CT of the abdomen showed gas in the pancreatic compartment (Fig. 2). An air-fluid level was seen above a collection of fluid measuring 80×50 mm (TxAP) in the omental sac (Fig. 3). Pneumoperitoneum and a small amount of free fluid in both paracolonic regions and perihepatic free fluid were also observed (Figs. 2 and 3).
The patient was admitted to intensive care with a diagnosis of emphysematous pancreatitis. Treatment was conservative using endoscopic techniques. An endoscopic transgastric drain was first placed. Five sessions of endoscopic necrosectomy were then performed in the first 30 days. In addition, a biliary prosthesis was placed as pancreatitis causes dilation of the bile ducts. A collection due to a biliary fistula was observed 20 days after the last necrosectomy, and so a second endoscopic drain was placed. The fistula eventually closed spontaneously without surgery.
Seven months after the episode of pancreatitis, resolution was complete and only a small nodular remnant of the pancreatic parenchyma remained. The causative agent in our case was Enterobacter aerogenes.
Figure 1. Simple abdominal x-ray (AP view) showing: intestinal fecal remains (white arrowheads). The lower border of the left renal silhouette (small white arrow) and absence of the right renal silhouette. The sentinel loop sign (small black arrow). The effacement of the left psoas line at its upper limit (long black arrow).
Figure 2. CT of the abdomen showing: gas in the pancreatic compartment and omental sac, with an absence of pancreatic parenchyma (white arrow). Edematous rest of the pancreatic body with the loss of its haustration (arrowhead), A small bubble of pneumoperitoneum in the anterior compartment (thick arrow). A small amount of intraperitoneal free fluid under the liver and in the posterior wall of the peritoneum (black arrows)
Figure 3. CT scan showing the collection with an air-fluid level in the omental sac (white arrow), pneumoperitoneum (thick arrows), and the edematous rest of the tail of pancreas (arrowhead).peritoneum (black arrows)
DISCUSSION
The presence of gas in the pancreatic bed is unusual. The most frequent causes are infected pseudocysts, abscesses, benign fistulas and malignant processes[1]. Emphysematous pancreatitis is a rare and serious complication of severe acute pancreatitis, in which pancreatic parenchyma necrosis occurs and the pancreas is replaced by gas. The condition has a high mortality rateas a result of sepsis[2]. Abdominal CT is the imaging test of choice as it has a high sensitivity and specificity for gas detection, and can also detect fluid collections, thrombosis or other complications (Fig. 3).
Some 80% of patients with acute pancreatitis have a mild form of the disease that does not require aggressive treatment. However, acute pancreatitis is a serious condition which can be lethal and whose incidence is increasing[2].
Oedematous pancreatitis is the most common form of acute pancreatitis, but approximately 10–20% of patients develop necrosis of the pancreatic parenchyma or peripancreatic tissues with sterile inflammation. In a third of this group, the necrotic tissue becomes infected[2], which is frequently associated with refractory sepsis and multiorgan failure. Deaths within the first 2 weeks are considered to be due to sepsis and multiorgan failure, while subsequent mortality is caused by necrosis or infected necrosis[3].
The treatment of severe acute pancreatitis requires a multidisciplinary and individualized approach based on:
- Supportive therapy for the prevention of complications
- Treatment of the causes
- Early and aggressive recognition of complications.
There are two possible approaches to emphysematous pancreatitis: conservative treatment which includes antibiotic therapy, percutaneous puncture and endoscopic techniques, and surgical debridement which can be open or laparoscopic.
The pucture of the necrosis allows us to treat according to the antibiogram. Thus, surgery is deferred, which allows necrosis organization, decreasing the morbidity and mortality of the surgery[4]. Late surgery is currently preferred because it results in less mortality compared with early surgery. Gas-producing bacteria are found in emphysematous pancreatitis, with Escherichia coli being the most common.
Although surgical necrosectomy is the treatment of choice[5], conservative management with endoscopic techniques allows drainage and necrosectomy with good results. In a multicentre study of patients with infected pancreatitis and necrosis, there were no significant differences in terms of mortality and serious complications between a group of 47 patients treated with percutaneous drainage and surgery, and 51 patients treated with endoscopic techniques[2]. The most frequent cause of mortality in both groups was sepsis followed by multiorgan failure[2]. In this study, the surgical technique applied was video-assisted retroperitoneal debridement (VARD), which is associated with fewer complications than open surgery[2]. Percutaneous drainage, which has a cure rate of 51%[2], is another option for the treatment of infected necrosis and is frequently used in combination with surgery or endoscopic techniques[2].
The severity and peculiarity of this disease require individualized and multidisciplinary treatment, requiring coordination between several departments and the combined use of several techniques.