Keywords
Tetanus, dysarthria, delayed diagnosis, computed tomography
Abstract
Introduction: Tetanus is a vaccine-preventable disease caused by a neurotoxin produced by Clostridium tetani that proliferates in wound sites. Toxin interference with neuromuscular function leads to spasms. Trismus, risus sardonicus and opisthotonus are classic features, but tetanus can begin with subtler symptoms.
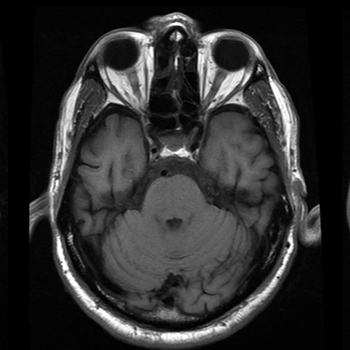
Case Description: An 80-year-old man presented with dysarthria. His medical history included hypertension and dyslipidaemia. No other neurological compromise was apparent on admission. Cranioencephalic computed tomography suggested pontine and mesencephalic ischaemia and stroke treatment was implemented. Two days later, the patient displayed dysphagia that required nasogastric intubation. The next day, he developed an apparent tonic seizure with respiratory distress refractory to diazepam and phenytoin, which required sedation and invasive mechanical ventilation. Ultimately, he manifested trismus and generalized spasms. Once the diagnosis of tetanus was established, he was given anti-tetanus immunoglobulin, tetanus toxoid vaccine and metronidazole. Magnetic resonance imaging did not reveal any brain injury. During his intensive care stay, he showed cardiovascular instability, developed nosocomial pneumonia, and required prolonged ventilator support and tracheostomy. He gradually improved during a 70-day hospital stay and regained his previous functional status.
Discussion: Dysarthria in an older patient with known cerebrovascular risk factors in addition to possible brainstem ischaemia contributed to an incorrect diagnosis of acute ischaemic stroke. Early manifestations of tetanus can mimic focal deficits. The limitations of brainstem computed tomography should be kept in mind.
Conclusion: Older patients present a broader range of signs suggesting tetanus, including a higher frequency of bulbar symptoms, on presentation. A careful anamnesis including previous vaccination history is key for identifying high-risk patients and to widen the differential diagnosis to include tetanus.
References