Keywords
Thrombosis, inferior vena cava syndrome, lumbar pain, nephroblastoma
Abstract
Inferior vena cava syndrome is rare and often difficult to diagnose because of its rarity and consequent low suspicion.
We describe the case of a 28-year-old female patient with a history of nephroblastoma of the right kidney, stage IV, with a favourable histology with epidural metastasis (D5-D9), diagnosed at 3 years of age. The patient underwent treatment with surgery, chemotherapy and radiotherapy.
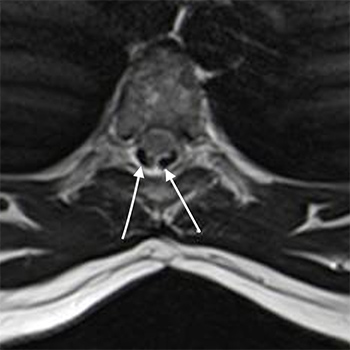
The patient suffered from sudden low back pain worsening over 2 weeks, with progressive inability to walk. The pain radiated to the front of the thighs. Concomitantly, oedema of the lower limbs with cephalocaudal progression was observed. At admission to our institution, the physical examination showed peripheral oedema, abdominal wall venous collaterals, an inability to walk due to low back pain in the supine position, with no neurological deficits. Lumbar MRI showed exuberant epidural venous congestion. The hypothesis of inferior vena cava thrombosis (IVCT) was considered and confirmed by angio-CT.
IVCT is prevalent in patients with congenital anomalies of the inferior vena cava, occurring in approximately 60–80% of these cases, and most published series on inferior vena cava syndrome refer to thrombotic complications in this subgroup of patients. There are currently no guidelines defined or validated to guide the diagnosis and approach to IVCT. With this case, we would like to draw attention to a rare disease that should be suspected in all patients with inferior vena cava disease, whether resulting from congenital disease or after surgical procedures.
References