Keywords
Warfarin resistance, genetic polymorphism, international normalized ratio, VKORC1, cytochrome P450
Abstract
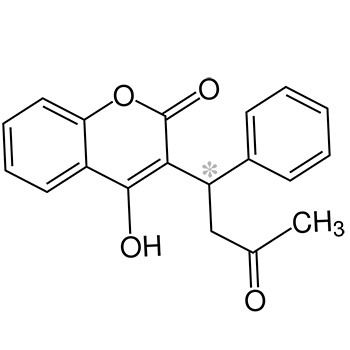
Warfarin is a readily available anticoagulant used worldwide in a variety of clinical scenarios. Patients who need more than 15 mg/day are considered to be warfarin resistant. Numerous genes have been implicated in warfarin pharmacogenetics, with genes encoding CYP2C9 and VKORC1 shown to be the most important determinants of drug dosage requirements. A 27-year-old woman was admitted as she had a sub-therapeutic international normalized ratio (INR) after prosthetic mitral valve replacement. Even after a warfarin dose of 50 mg/day, her INR was not in the therapeutic range, so the heart team decided to replace her metallic valve with a bioprosthetic valve, thus alleviating the need for anticoagulation.
References