Keywords
infective endocarditis, NSAIDs, diclofenac, mycotic aneurysm, haemorrhagic stroke
Abstract
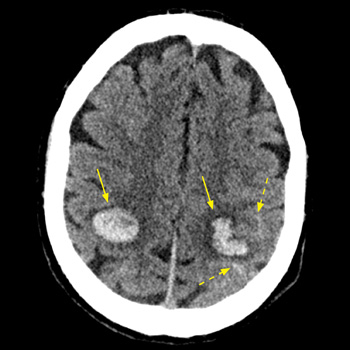
Introduction: Intracranial haemorrhage may complicate infective endocarditis, caused by ruptured mycotic aneurysms or haemorrhagic transformation of brain septic emboli. The risk of intracranial bleeding may increase with the use of non-steroidal anti-inflammatory agent (NSAIDs).
Case description: We report on a 53-year-old male patient with a past history of intravenous drug abuse, who was treated with diclofenac (75 mg IM) for a few hours of preceding fever and arthralgia. Seven hours later he was hospitalised with impaired consciousness and hemiparesis. Evaluation revealed multiple intracranial haemorrhages, at least one originating from a mycotic aneurysm. Repeated blood cultures grew methicillin-resistant Staphylococcus aureus (MRSA), and echocardiography revealed a vegetation on the mitral valve, establishing the diagnosis of bacterial endocarditis.
Conclusion: The abrupt simultaneous multifocal intracranial bleeds shortly following the administration of NSAIDs for a few hours of febrile disease, one clearly originating from a mycotic aneurism, are exceptional. This raises a possibility of a role for diclofenac the intracranial bleeding diathesis in this unique clinical presentation. Intracranial haemorrhage in the set-up of undiagnosed infective endocarditis (IE) might be added to the long list of potential adverse outcomes of NSAID administration, and the possibility of IE should be considered before their administration for febrile disease of undetermined cause.
References
Views: 316
HTML downloads: 37
PDF downloads: 275
Published:
2023-09-05
Issue:
2023: Vol 10 No 10
(view)