Keywords
Clostridioides difficile, abscess, intraabdominal, extraintestinal
Abstract
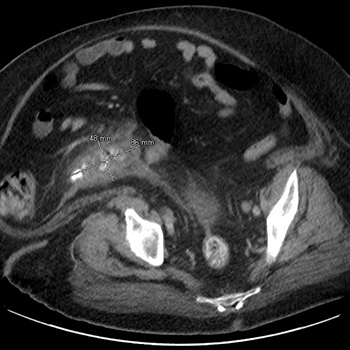
Clostridioides difficile infection (CDI) commonly presents with diarrhoea, colitis, and in more severe cases, toxic megacolon. Extraintestinal Clostridioides difficile infection (EI CDI) is rarely reported. Intraabdominal abscesses are the most commonly reported EI CDI presentation. EI CDI-associated bacteraemia, as well as bone, lung, and even intracranial infections have been reported in the literature. EI CDI is usually seen in patients with multiple comorbidities. Due to the rarity of cases, no clear treatment guidelines exist, but metronidazole and vancomycin have been primarily used to treat EI CDI and additional antibiotics have been used for treatment when the isolates are polymicrobial. We report a case of a patient with significant comorbidities who developed EI CDI following acute ruptured appendicitis. She was successfully treated with drainage of abscess and intravenous metronidazole followed by oral metronidazole.
References