Keywords
High-risk pulmonary thromboembolism, alteplase, systemic thrombolysis
Abstract
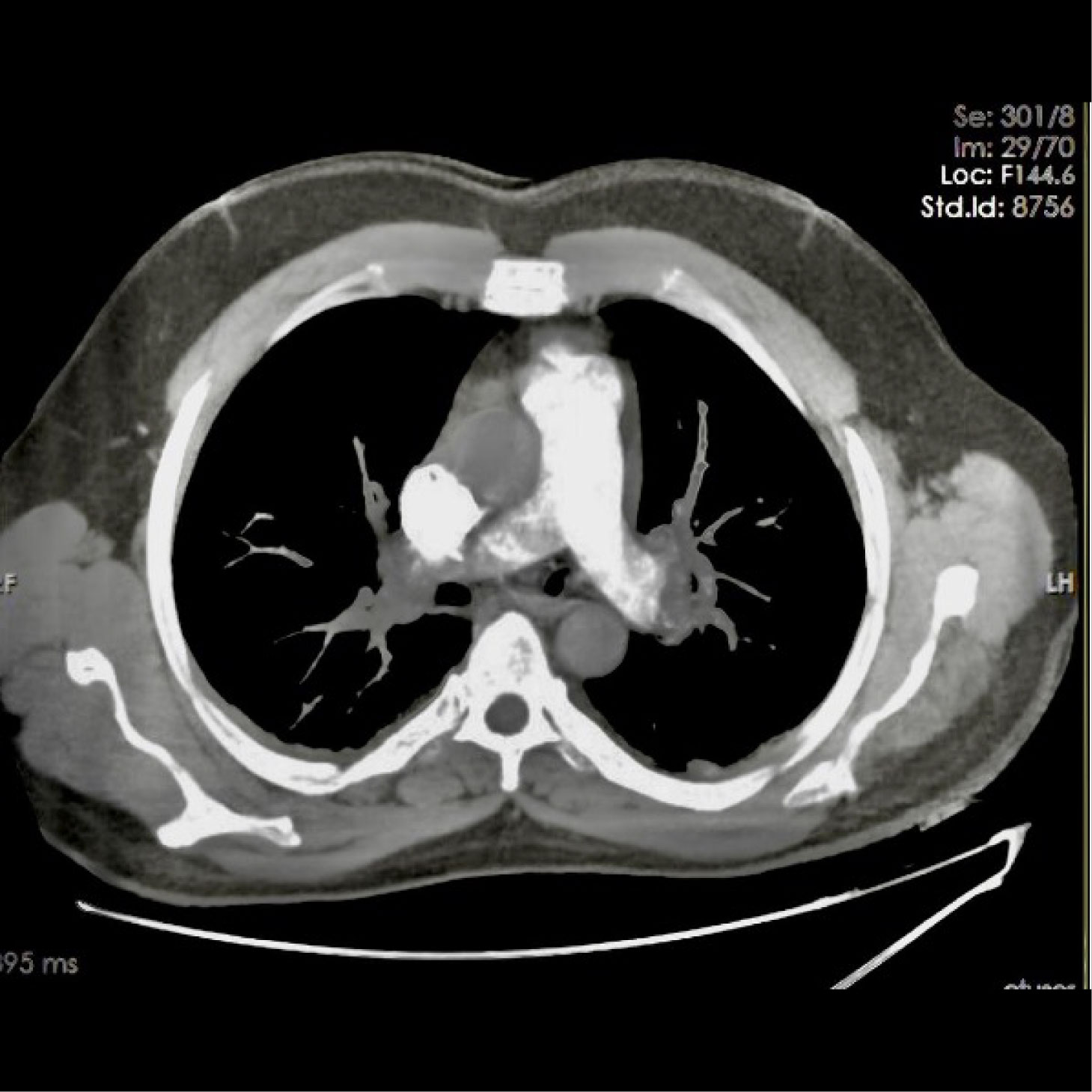
Acute pulmonary thromboembolism (PTE) is considered the third most frequent acute cardiovascular syndrome behind myocardial infarction and stroke, with annual incidence rates ranging from 39 to 115 per 100,000 people and ranking high among the causes of cardiovascular mortality. High-risk PTE is characterised by haemodynamic instability and encompasses clinical manifestations such as cardiac arrest, obstructive shock and persistent hypotension. The European Society of Cardiology (ESC) recommends a reperfusion strategy with systemic thrombolytic therapy for high-risk PTE under class I, level B if there are no contraindications. Overall, unsuccessful thrombolytic therapy and recurrent PTE have been reported in 8% of patients with high-risk PTE. The guidelines recommend surgical pulmonary embolectomy if thrombolysis is contraindicated or has failed. The position of repeated thrombolytic therapy as a treatment option in patients with recurrent high-risk PTE, especially in situations with a lack of surgical expertise or resources, was not mentioned in the guidelines. We report the case of a patient who suffered a recurrent high-risk PTE and was treated with repeated thrombolytic therapy that was effective and resulted in excellent outcomes.
References
Views: 433
HTML downloads: 52
PDF downloads: 336
Published:
2023-08-25
Issue:
2023: Vol 10 No 9
(view)